Search
-
What it's Really Like to Have a Mammogram
Have you found yourself avoiding scheduling a mammogram because it sounds uncomfortable and maybe a little scary? Many people feel this way but knowing what to expect can help ease your worries. Follow along for a reassuring step-by-step guide on getting a mammogram from Melissa Dahir, Community Relations Liaison at Renown Health. Getting a mammogram is important to me because my mom is a Stage 3, double mastectomy breast cancer survivor. I began receiving annual breast health screenings at an early age, in addition to performing monthly self-exams. So far, all my appointments have gone well, and I hope that sharing my experience will encourage you to schedule this important screening today! Scheduling the Appointment Scheduling my appointment was very easy. I contacted the scheduling team for help with booking multiple appointments and they were very helpful in finding just the time I needed.
-
Department Spotlight: Hospice & Palliative Care
In the book of life, everyone eventually reaches the final chapter. End-of-life isn’t often something a patient or loved one wants to think about. The end of someone’s life isn’t a final option – it's a privilege. At Renown Health, we have a compassionate team prepared to approach this privilege with kindness and care. The Hospice & Palliative Care department at Renown is the best of the best. Their efforts go far beyond simply addressing physical pain; they also bring emotional and spiritual solace to patients and family members navigating the complexities of serious illness and end-of-life. This team provides crucial guidance and expert knowledge, comfort and care when it is most needed. Bringing Dignity to the Final Days Contrary to popular belief, hospice and palliative care is not a “last resort” option for families. In fact, it’s quite the opposite. These caring professionals work hard to ensure a patient’s final days are free of pain and full of peace, rather than focused on the end. This type of care isn’t a death sentence – it's a living gift. Each patient is involved in his or her own end-of-life process. They have a huge role in deciding on their own and with their family members how they want to live out their remaining days. “Every team member’s daily work focuses on how to facilitate a good death for each patient,” said Tanya Prosch, Hospice Supervisor. “Ultimately, it is up to each patient’s family to be involved in this process. Every day, there is a lot of communication among team members as we prioritize the needs of our patients. As patients decline and their symptoms change, we continuously assess what topics we will discuss. This creates a beautiful back-and-forth dynamic among the team, patients and families.” “Together, we come as a team to provide what they need, ensuring individualized care for each patient and family based on their safety and specific needs,” added Rachel Schneider, Transitional Care Specialist. “Our care plans are not cookie-cutter; they are tailored to fit each unique situation.” The hospice team provides comfort and support to those in the final stages of a terminal illness. Hospice is focused on one main goal, which is enhancing quality of life for patients and their families. “In general, hospice staff conduct home visits to see our hospice patients,” said Amy Nieminen, Manager of Home Health & Hospice. “We have an interdisciplinary team that includes nurses, aides, chaplains, social workers and volunteers. Together, we address both the physical and emotional, spiritual and social needs of our patients and their families at the end of life, ensuring they have a meaningful and peaceful experience. We do a lot of work with families and loved ones, providing follow-up calls and support for the patient’s caregivers after their passing. Our support extends for up to a year, with grief specialists available to help families through their loss. Additionally, we have rotating on-call nurses every night and weekend, so patients are never left without care.” While palliative care shares similar duties to hospice care, it differs slightly. Palliative care can be involved at any stage of a serious illness, even during treatments. “During in-home palliative care, we work with patients who may be physically ready for hospice but who are not yet psychologically, emotionally or spiritually prepared to make that transition,” said April Lennon, APRN for In-Home Palliative Care. “They may still be exploring treatment options and working with their specialists. We provide a lot of support, helping them understand the consequences and benefits of various treatments. Additionally, we focus on symptom management for patients experiencing significant pain or nausea, assisting them in managing these symptoms effectively.” On both sides of this department, the team has the opportunity to be especially involved in their patients’ lives and in the lives of their families. Giving loved ones more time with their relative facing end-of-life is a duty that these team members take seriously. “My job is to educate families about what’s coming next and what is happening now, as there is a lot that occurs during the death process,” said Katie Adams, Hospice Nurse Case Manager. “Families will never regret the time and effort spent during this process. We have only one chance to get this right. This is not just a random hospitalization that people will forget; it is a significant moment that everyone around the patient will remember.” “Being able to connect more deeply with patients’ and families’ stories and their narratives about life is essential, as it provides a broader understanding beyond just the medical picture of what is happening,” added Libby Krayk, APRN for Hospice. “We explore their expanded value and belief systems to assist with decision-making, helping them make choices together. When patients are no longer distracted by pain or nausea, they can focus on their long-term desires and goals and spend more time with their families." “Crisis intervention, social work, education, family conferences, and placement issues are all part of what we do, and it’s quite exciting,” added Donald Kamka, Social Work Care Coordinator. “You become fully invested in the lives of those you help, which is what makes this job so rewarding. This is a remarkable time in their journey, and it’s evident that everyone involved has a vested interest in it." Naturally, many questions, worries and fears arise during this time in a patient’s life. The Hospice & Palliative Care team members are expert communicators and know exactly how to relieve some of those anxieties, prompting a more peaceful end-of-life. According to this team, it’s all about transparency and compassion. “Our role involves helping patients navigate the healthcare system as they face death,” said April Lennon. “Home visits can range from one hour to three hours, depending on the needs of the patient and their family. We engage with entire families, including those who are out of town, coordinating care and working with many providers in the area. Our hope and goal for every patient is to ensure they understand what they are doing and why they are doing it, empowering them to make their own choices.” “We often find ourselves addressing the most difficult information, which can sometimes be seen as the ‘elephant in the room’ that people tend to avoid,” added Libby Krayk. “I ask patients for their permission regarding what they want to know and who they would like involved in the conversation. This approach can help alleviate some of the challenges and stress they may be experiencing. Being honest and discussing matters in a way that they can understand is essential. I take the time to sit down with my patients and connect with them on a human level, rather than just a medical level.” As a not-for-profit health system, volunteers are at the core of our mission delivery. They graciously dedicate hours out of their week to be a friendly source of help for patients. Renown’s Hospice Volunteers exude this level of kindness and more. Our employed team members attribute their volunteers as a major source of success for Renown’s hospice program. “I believe that being a volunteer provides a role that patients perceive as non-threatening,” said Linda Derry, Hospice Volunteer. “As volunteers, patients feel more comfortable talking to us and sharing things. This dynamic allows them the freedom to express not only how they are feeling but also their fears and any other concerns they may have. It is in these moments that we can truly connect with them, as we are volunteering out of a genuine desire to sit and visit with the patients. “When I see a patient, the focus depends on their specific needs,” added Luanne Geissler, Hospice Volunteer. “I often give family members some time to themselves to do whatever they need to do while I visit with the patient. Many of them are very talkative and eager to share their stories. For instance, one patient told me how to make a baked potato while out in the wilderness, which has become one of my favorite stories. Another patient shared her experiences about coming to America from Asia, discussing her church, her religion and her passion for baking. She would even bring bread to her doctor.” “I have one patient whose main desire is to play chess; he has been playing for over 80 years and is still able to play very well,” added Hervey Ibarra, Hospice Volunteer. “When I visit another patient at his home, we engage in conversations about a variety of topics. Additionally, some patients ask me questions about the military and law enforcement. Whatever they want to do and discuss, that is what I focus on during our time together.” Regardless of whether they are a provider, supporting team member or a volunteer, every person on the Hospice & Palliative Care team shares a primary focus: helping patients live their remaining days, no matter how long that may be, with dignity and comfort, surrounded by their loved ones.
Read More About Department Spotlight: Hospice & Palliative Care
-
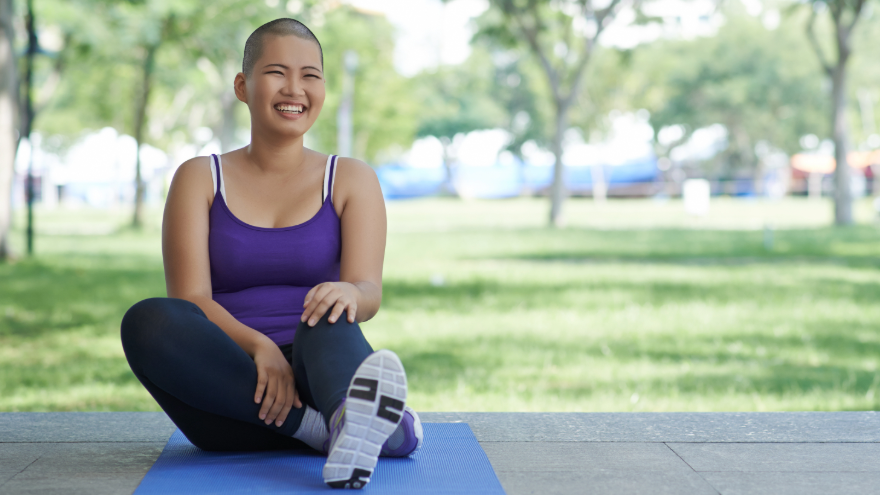
Can Exercise Really Help Prevent and Heal Cancer?
Did you know that being physically active can lower your risk of developing at least thirteen different types of cancer? Exercise plays an important role in preventing and recovering from a cancer diagnosis. Not only does it have a positive impact on building your body’s strength, but physical activity can also help you with your mental well-being and boost your quality of life. For the first time, the American Cancer Society (ACS) projects that U.S. cancer cases will surpass 2 million in 2024. With cancer cases on the rise, help reduce your risk by being proactive about your health. Below, discover how exercise can help you reduce your risk of cancer, assist you on the road to recovery when undergoing treatments, and move forward with a healthy, cancer-free future. How Exercise Helps Fight Cancer A healthy diet and lifestyle have a direct link to cancer prevention, and physical activity has been proven to lower the risk for several types of cancer. The Centers for Disease Control and Prevention (CDC) reports that obesity and being overweight make up 40% of all cancer cases in the U.S. each year, increasing your risk for 13 different kinds of cancer. This accounts for more than 684,000 cancer cases in the U.S. each year. According to the ACS, physical activity has been linked to a lower risk of several types of cancer, including: Colon cancer (for which the link is strongest) Breast cancer Endometrial cancer (cancer in the lining of the uterus) Bladder cancer Esophagus cancer Stomach cancer Physical activity might also affect the risk of other cancers, such as: Lung cancer Head and neck cancers Liver cancer Pancreas cancer Prostate cancer Ovarian cancer Research shows that exercise can help to prevent cancers by: Controlling weight and preventing obesity. Reducing sex hormones or insulin. Strengthening the immune and digestive system.
Read More About Can Exercise Really Help Prevent and Heal Cancer?
-
Why Mammograms Are Vital for Early Breast Cancer Detection | Renown Health
Breast cancer affects 1 in 8 women in the U.S. each year, making early detection crucial in improving the chances of successful treatment. Early Detection for Treatment and Peace of Mind Mammograms are noninvasive X-rays used to detect cancer and other abnormalities in the breast. They are the most effective screening tool for detecting breast cancer early, allowing for timely treatment before the disease can spread and helping to improve treatment outcomes. To help guide you through the mammogram process, we spoke with Elizabeth Kang, PA-C, at Renown Breast Surgery Care to equip you with expert knowledge on what to expect and why screening is so important. How Accurate are Mammograms? 3-D mammography technology at Renown Breast Health Center can detect 41% more cancers and reduce the number of false-positive results compared to plain film mammography. Benefits of 3-D mammography include: Providing better, clearer images, with higher diagnostic accuracy Allowing radiologists to see more abnormalities in the breast Helping doctors spot more cancers and avoid false positives, especially if you have dense breast tissue Reduced callback rates for findings on screening Mammogram Screening and Breast Exam Recommendations Renown Women's Health recommends the following breast exam guidelines: Age 18-39: Consult your primary care provider for a Risk Assessment and start breast exams at age 25. Age 40+: Get your annual mammograms. Family history: Begin screening 10 years before your youngest family member's age at diagnosis. For example, start at age 35 if a family member was diagnosed at 45. Self-awareness: Be familiar with the look and feel of your breasts and report any changes to your care provider. Age 75+: Continue annual mammograms if life expectancy exceeds five to seven years. What screenings are available for women with breast implants? Women with breast implants can and should still receive mammograms, and it’s essential to have these screenings done by an experienced team. Be sure to inform your healthcare provider and mammogram technicians about your implants, as they may recommend special techniques or steps to detect abnormalities and ensure accurate results.
Read More About Why Mammograms Are Vital for Early Breast Cancer Detection | Renown Health
-
7 Symptoms of Breast Cancer in Young Women
Cancer can develop at any age, and that’s why the experts at Renown are ready to help you stay ahead of breast cancer, especially if you're in your 20s or 30s. We're talking about early detection, signs to be aware of, and why being proactive is a big deal. Studies show there has been an increase in breast cancer in younger women. Although breast cancer is rare in women under 40, when it occurs, it tends to be aggressive. The tricky part? Many young women don't think it can happen to them, so they don't check for the signs as often as they should. Reviewed by Dr. Colleen O'Kelly-Priddy, MD, FACS, breast surgical oncologist at Renown Women's Health. Early Signs and Symptoms New or Different Lump in the Breast: A lump is probably the most well-known symptom. Breast cancer is usually painless and firm, but it can also be soft. If you find a new lump, don't panic, but don't ignore it either. Changes in Breast Size or Shape: Have you noticed that one breast looks a little different? Whether it's swelling, shrinking, bulging, dimpling, or seems off, it's worth mentioning to your doctor. Skin Changes: If the skin on your breast starts to thicken or turn red, it's time to pay attention. If your skin starts looking like an orange peel (thickened, with prominent pores), that warrants evaluation. Nipple Discharge: Spontaneous drainage coming from your nipple that isn't breast milk—especially if it's clear or bloody—should be checked out. Nipple Changes: If your nipple starts to invert, flatten, or look different, call your doctor. Breast Pain: Continuous pain in your breast or nipple that isn't linked to your menstrual cycle is another symptom to note. However, breast pain is very common and is only rarely a sign of cancer, so don’t panic. Swelling or Lumps in the Armpit: When it spreads, breast cancer usually first goes to the lymph nodes in the armpit, so swelling or lumps under your arm should be on your radar.
-
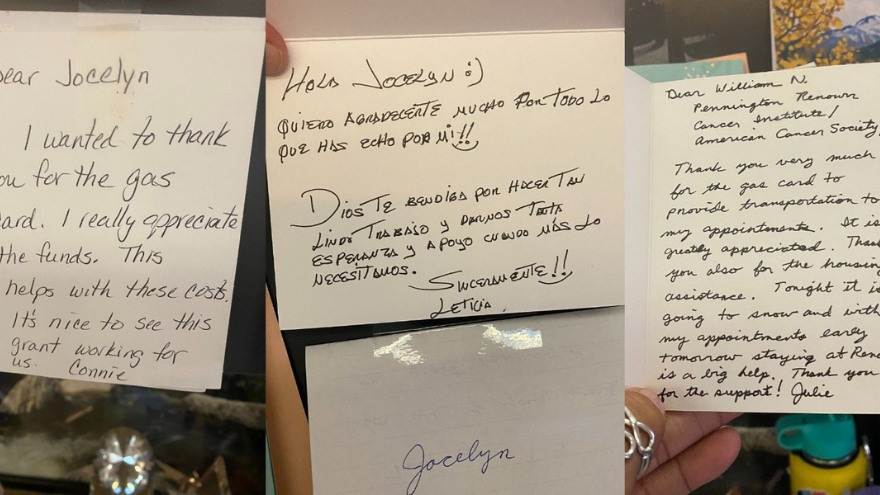
A Journey of Support: How Grants from the American Cancer Society Impact Patients at Renown
For many cancer patients, a significant hurdle is simply getting to treatment. Patients from Nevada and California often face considerable financial and logistical challenges when traveling for care. Limited resources for transportation and lodging can result in missed appointments, treatment interruptions and delays in follow-up care. To address this crucial need, Renown Health Foundation partners with the American Cancer Society (ACS) to ensure our patients can access the care they need by reducing financial barriers many patients face ACS awarded $70,000 to Renown Health Foundation last year. These funds, distributed as gas cards and lodging support to qualifying patients, have proven to be a lifeline in assisting those in need. Fueling Hope with Gas Cards Through our partnership with ACS, Renown supported 128 cancer patients over the past year. This assistance provided 2,260 round trips, ensuring that patients from Nevada and California could attend their critical treatments at the William N. Pennington Cancer Institute at Renown. These patients, aged 15 to 94, traveled up to 320 miles, sometimes from remote areas such as Tonopah, Elko and Susanville, for their cancer care “We're deeply committed to supporting our patients through every step of their journey, and our partnership with the American Cancer Society is instrumental in making that happen,” said Jocelyn Mata, Oncology Social Worker at the Pennington Cancer Institute. “Without them, we wouldn't be able to provide the crucial financial assistance that many of our patients need.” Jocelyn works with qualifying patients to provide gas cards and accommodations at The Inn at Renown, a hotel at Renown Regional Medical Center. She ensures they can focus on their treatment without worrying about the financial burden. Lodging Support for Peace of Mind Along with transportation aid, we can provide safe and comfortable lodging for qualifying patients. "We encourage patients to rest and, if they have a long journey home, to stay overnight," said Dr. Max Coppes, Director of the William N. Pennington Cancer Institute. "Providing lodging support ensures they have a safe and comfortable place to recover before making the trip back." This assistance is crucial for those who travel far from home, allowing them to focus on healing without the added stress of finding and affording accommodation.
-
From Patient to PAR: Jodee’s Road to Renown
When faced with chronic pain, that agonizing feeling of dread can be overwhelming to anyone, let alone a cancer survivor. Take Renown Patient Access Representative (PAR) Jodee Elder, for example. As she was receiving radiation treatments while Fighting the Good Fight against cancer, she started to experience pain at the base of her spine that ended up progressing to lower spine arthritis. On top of trying to beat cancer, the last thing she needed to deal with was the intense pain that was affecting her everyday life – and she deserved a solution that was going to provide her with the relief she needed for the long term. That’s where the Special Procedures – Pain Management department at Renown Rehabilitation Hospital – a part of Renown Spine, Sports & Pain Management – stepped in. But the team of doctors, nurses and imaging technologists Special Procedures had more on their minds for Jodee beyond pain relief. As a Renown employee, they knew what a best-in-class PAR Jodee was in her unit at the time, and they wanted that level of passion as the face of their department. Little did they know that Jodee shared the exact same sentiments. From Patient... As a skilled Patient Access team member since 2018, Jodee knows first-hand how important it is to set patients up for success before, during and after an intimidating procedure. She began her Renown career as a Pre-Registration PAR, eventually taking her expertise to Surgical Preadmission. During her years on those two teams, she honed her craft as a personable, patient-facing guide, continually going above and beyond for every patient and employee. But there was one problem: the chronic pain in her lower back that happened as a result of her radiation treatments. This pain ended up being diagnosed as lumbar spondylosis, a degenerative spinal condition that causes arthritis in the back. And when you work a desk job, back pain can be especially excruciating. When 2023 rolled in, Jodee knew she needed to try something new for her pain, something that would give her relief once and for all. After some research and advice from her doctor, she learned about Special Procedures, a team at Renown Rehabilitation Hospital offering pain management options that she wasn’t previously familiar with. Eventually, her care teams discovered that a bilateral radiofrequency nerve ablation may give her the relief she needed. Throughout the entire process, Jodee recalls feeling supported every step of the way with an experience personalized just for her. Despite being nervous at first, she was quickly put at ease by the caring nature of her pain management team. “From scheduling and the pre-operative process to the procedure and recovery experience, I often think about the amazing care I received from the entire team,” said Jodee. “Dr. Casey Keating and the nurses were with me at every point of my procedure. This was such a personal experience. I was treated like I was their only patient for the day, and everyone tried hard to alleviate any anxiety, stress or worries I had by comforting me with things like music, rubbing my leg and one-on-one conversations throughout the process.” Since her procedure, Jodee has been virtually pain-free, happily noting that she hasn’t taken any pain relievers from that day on. She gained a lot of coping skills from her care team that, as fate would have it, would inspire her to help other patients who are preparing for their own procedures. ...To Pain Management Patient Access... Before her first procedure even began, Dr. Keating was already told all about Jodee by a former coworker, who applauded her organizational skills. He very quickly was impressed by her work ethic and experience as a PAR. While she was undergoing her procedure, Jodee couldn’t help but notice how the nurses went above-and-beyond for her and treated her like she was a part of the team – even before they knew her. She immediately felt at home in Special Procedures, not only because of the level of care the team provided but also because of how much her life changed after receiving the much-needed relief for her back pain. “When I came for my first injection, Dr. Keating introduced me to the nurses as ‘the PAR we want over here,’” said Jodee. “I was on the fence regarding leaving my current PAR role, but after my experience with Special Procedures, the team really sold me on the opportunity. I immediately thought, ‘I want to be a part of this.' They were so appreciative of me from the start." And the rest is history. On Nov. 17, 2023, Jodee began her journey as the PAR dedicated solely to Special Procedures. On a typical day, you can find Jodee interacting with patients ahead of time to make checking in more enjoyable, helping patients through the pre-registration process, scheduling our Renown-employed and community providers for each procedure, checking up on authorizations, and of course, leaving a positive impact on everyone she connects with. In addition, she is known as the Special Procedures “chart master” as the main employee organizing each patient’s chart. But her duties as a PAR go beyond the desk. As a former patient herself, she has the unique ability to relate to Special Procedures patients who are worried and anxious about the road ahead. “When nervous patients come in, I can connect with them on a personal level and support them with suggestions that helped me out when I was going through my procedure,” said Jodee. “I love being patient-facing. You wouldn’t believe how many patients we’ve helped enter their procedures calmer than they were before and get the relief they need. I enjoy taking care of these patients – that's why I got into healthcare. I wanted to make a difference.” ...And Beyond Today, Jodee has been a proud PAR in Special Procedures for almost a year. She has thoroughly enjoyed her time with her fellow team members, who have been nothing short of a family to her in more ways than one. “This team is incredibly supportive of me both at work and in my personal life,” said Jodee. “When my mother passed away, they sent me a beautiful flower arrangement and a card that they all signed. The day I came back to work, they all hugged me and said they were always there for me if I wanted to talk. It’s like a big family here.” In her experience as a patient and a PAR, Jodee lives by one main motto: start a chain reaction. As she emphasizes, it only takes one of us to start a chain reaction to affect patients and the community. In Special Procedures, it starts with Jodee. And in life, she tells her kids to be that chain reaction starter. Outside of work, Jodee enjoys spending time with her kids and is happily anticipating the arrival of her grandson, who was conceived very close to the day that her mother passed away. She always makes time to create new memories with her family, including “tattoo roulettes,” where they each put a few tattoo ideas in a hat and pick one at random; they then go out and each get matching tattoos as a testament to their love for one another. “When one life ends, another life blooms,” said Jodee. If you are interested in receiving care with Renown Spine, Sports & Pain Management, speak with your provider about a referral to our specialized team. In the meantime, we encourage you to learn more about navigating your pain management care with Renown Health.
-
How to Get Started and Make Updates to Your Will
August is National Make-a-Will Month. We talked to Abbey Stephenson, Planned Giving Officer at Renown Health Foundation, to learn more about wills, trusts and estate plans and why you should feel motivated this month to get started. Why Make a Will There are so many reasons why it is difficult to make a will or put an estate plan in place. These include: Lack of time or money to prepare a plan The misperception that “only rich people need an ‘estate plan’” How intimidating legal documents can be General discomfort with planning for the future Given the barriers to making a plan, it’s not surprising that only 32% of Americans have a will or trust in place. But having a will or trust matters because these are the documents where you can say who will inherit your assets, who will manage your assets and estate, and who should be guardian of a minor or a child with a disability. Where to Begin If you have been thinking about putting together a will and don’t know where to begin, here are some next steps you can take. 1. Learn the terms. If you have never created a will, trust, or an estate plan, the language can be hard to get used to. A few important terms to know include: Last will and testament (also known as a will): a legal document that describes how you would like your property and other assets to be distributed after your death. This is also the document where you can nominate a guardian for a minor or disabled child. Personal representative (also known as an executor): a person named in a will responsible for collecting your assets, paying your debts and final taxes, and distributing the remaining assets to those stated in your will. Personal representatives must be formally appointed by a judge and report certain information to the judge for review and approval. Living trust (also known as a revocable or family trust): a legal arrangement set up through a document called a trust instrument or a declaration of trust that gives someone called the trustee power to make decisions about the trust creator’s money or property held in the trust. Estate plan: a collection of documents that help organize what happens to you and your assets upon your disability and death. Your estate plan is comprised of documents such as a will, trust, and advance health care directive. If you want to learn more about these terms and estate planning in general, you are invited to attend a free one-hour estate planning education session on Aug. 22, 2024, at 10 a.m. or Oct. 21, 2024, at 11 a.m., hosted by Renown Health Foundation. Click here for more information and to register. 2. Create a list of assets. Start by creating a list of your assets including real estate, investments, bank accounts, retirement accounts, business ownership interests, vehicles, life insurance, valuable personal property like jewelry or artwork, and any other significant assets. Click here and read our free estate planning guide. 3. Put together a list of 2-3 people you trust. When you create your will, you need to name a personal representative who will collect all your assets, pay your debts, and work with the probate court to distribute the balance to the people and charities you name in your will. If you create a trust, you need to name a trustee to manage the trust assets under the terms of the trust document. It is a good idea to include at least two people who can take on these roles in case the first person becomes unavailable. If you do not have anyone you would trust as a personal representative or trustee, there are trust companies, banks, and other professionals and institutions who may be able to assist you. If you are the parent of a child who is under 18 or has a disability, you will also nominate a guardian in your will to care for that child if you and the other parent are gone. 4. Start a list of who you would like to inherit your assets. Which people and organizations would you like to inherit the assets you own at the time of your passing? And which assets or how much would you like them to receive? You might want to consider who relies on you for support such as family members or charities, individuals and organizations that have made a difference in your life, or those you have a special fondness for. It is important to use the legal names of individuals you include as beneficiaries and the Tax ID number for any charity you include. If you decide to make a gift to Renown as part of your will or estate plan and notify us, you will be included in the Renown Legacy Society. Legacy Society members enjoy invitations to exclusive events, special acknowledgments, and other unique benefits. Click here to learn more about the Renown Legacy Society. 5. Put together a list of your professional advisors and enlist their help. Write down the names and contact details for any professional advisors you work with such as your accountant, financial advisor, investment manager, attorney, insurance agent, and planned giving officer. You may want to seek their advice on how best to proceed and which assets are best gifted to which individuals and organizations from a tax standpoint. Collaboration among the professionals with whom you work can help your plan to run more smoothly when it is needed. Depending on your circumstances, it may make sense for you to introduce your trusted individuals to these professionals. 6. Start drafting. Once you have these items in place, you will be in a good position to begin the drafting process. There are many capable estate planning attorneys in our community who can help you with drafting. There are other drafting resources available as well, but only a licensed attorney can provide you with legal advice. Click here to attend the free Family Estate Planning Series sponsored by Renown and presented by PBS Reno and the Community Foundation of Northern Nevada.
Read More About How to Get Started and Make Updates to Your Will
-
How Diet Can Affect Cancer Risk and Recovery
Cancer affects millions of lives worldwide. Though medical advancement has done a great deal to increase the human lifespan, proper nutrition has also been proven to help in the prevention of cancer. As researchers continue their hunt for a cure, there is a lot of information out there to support the argument that nutrition is an essential component in disease prevention and management. Nutrition Services: To learn more, call us at 775-982-4000 Linking Diet and Cancer Risk Evidence shows that our diets impact our vulnerability to cancer – and our ability to fight it. The American Cancer Society states that at least 18% of all cancers in the United States are related to excess body weight, physical inactivity, alcohol consumption, and/or poor nutrition. (American Cancer Society Guideline for Diet and Physical Activity | American Cancer Society). Sure, genetics can contribute, but research continues to support the belief that following a healthy diet can reduce the likelihood of developing cancer in the first place. Renown Health’s Jessica Blauenstein, MS, RDN, LDN, CSO, Registered Dietitian and Board-Certified Specialist in Oncology Nutrition confirms the importance of a nutritious diet consisting of: Fruits and Vegetables: Eating a variety of fruits and vegetables provides large amounts of vitamins, minerals and antioxidants. Nutrient-rich, they help in fighting off oxidative stress and inflammation, both of which are factors for developing cancer. Whole Grains: A diet rich in grains such as brown rice, quinoa and oats, contains substantial amounts of fiber that helps in digestion. A few studies have shown that whole grains might offer some protection against colorectal cancer. Lean Proteins: Reducing the amount of red and processed meats in the diet by substituting lean proteins, such as poultry, fish, beans and lentils may lower the risk of developing cancer. Red and processed meats have been associated with colorectal and other cancers when consumed in large amounts. Healthy Fats: Begin focusing on healthy fats from foods like avocados, nuts, seeds and olive oil. These fats are anti-inflammatory, which may play a beneficial role in disease prevention. Avoidance of Sugar and Processed Foods: Sugar and foods high in processed ingredients have been linked to an increased risk of obesity, type 2 diabetes and some cancers. It's important to limit the intake of sugary drinks, candy and snacks in the battle against cancer. A Role of Nutrition in Cancer Recovery Nutrition becomes even more critical for individuals who receive treatment and are in recovery. Treatments such as chemotherapy, radiation therapy and surgery can take a lot out of a body, affecting appetite, digestion and nutrient absorption. Proper nutrition during and after treatment can help: Support Immune Function: A good, balanced diet will provide the essential nutrients that support a resilient immune system, which is important in fighting off infections and supporting overall health during cancer treatment. Maintain Strength and Energy Levels: Proper caloric intake, protein and micronutrients prevent muscle wasting and fatigue, allowing patients to sustain their strength and energy. Address Side Effects: Certain foods and diets can help reduce or alleviate some common side effects associated with cancer treatment, including nausea, vomiting and mucositis. Eating small, frequent meals, maintaining good hydration, and avoiding spicy or acidic foods can all ease treatment-related discomfort associated with the GI tract. Facilitate Healing and Recovery: Nutrient-rich foods promote healing and the repair of tissues that may be damaged after surgery or other medical interventions. Foods high in proteins, vitamins and minerals play a significant role in repairing and replacing damaged tissues and cells. Correct Nutritional Deficiencies: Cancer and its treatment cause vitamin D, vitamin B12 and iron deficiencies in the diet. Nutrition therapy through a registered dietitian or nutritionist can identify those deficiencies and help manage them through dietary changes or supplementary means. Related information: Nourishing Your Loved One Through Cancer Treatment
Read More About How Diet Can Affect Cancer Risk and Recovery
-
Department Spotlight: Core Laboratory at Renown Regional Medical Center
When it comes to your health, tests are not only common but often also required to receive the most ideal treatment plan. From your routine urinalysis to more complex hematology cases, these tests help open the doors to proper diagnosis. Thousands of patients are seen at Renown Regional Medical Center every year, which results in thousands of lab samples needing to be processed every day. So, who rises to the occasion? Answer: The Core Laboratory team at Renown Regional. With the largest lab workload in our health system, the Renown Regional Core Lab is where compassionate care meets scientific excellence. While under the care of the Core Lab Team, patients can rest assured that they are in the greatest of hands - literally and figuratively - with every scientist, technical specialist and lab assistant that serves in this department. A Core Mission of Accuracy and Precision At Renown Regional, the only Level II Trauma Center in the region, the Core Laboratory works on a wide variety of lab tests to help providers diagnose, treat and monitor each patient’s condition. Those testing processes, known as “benches,” include: Blood Gas Chemistry & Immunoassay Coagulation Hematology & Differentials Urinalysis Working together in harmony, each member of the Core Lab team has an equally vital role in our health system, and all share a common goal. “Our number one priority is to provide accurate results for our patients, ensuring that the providers have all the correct information they need to treat them,” said Lauren Anderson, Manager of Core Laboratory. As one can imagine, there are several factors involved when it comes to ensuring those accurate patient lab results that Lauren mentioned above. “Throughout the day in the core laboratory, there are many tasks to be performed for the accuracy and validity of our patient results,” said Jackie Blazquez, Sr. Medical Lab Scientist. “The medical lab scientists perform maintenance on the instruments daily while accommodating patient samples and releasing results. Our clinical lab assistants help the scientists with receiving samples, reviewing patient labels for any discrepancies, answering phone calls and assisting with the automated lab sample line.” “The roles and responsibilities will vary depending on the bench assignment, but every bench will have one responsibility in common: performing preventative maintenance on our analyzers and running quality controls afterwards,” added Brittany Oliver-Stergiou, Medical Lab Scientist. From start to finish, there is rarely a dull moment in Renown Regional’s Core Lab. In fact, this capable team can process up to 7,000 samples per day at this hospital alone. "As a Medical Lab Scientist, for each instrument we use, we have to perform maintenance, calibration and quality control to ensure that the analyzer is ready for patient testing,” said Lauren Anderson. “Once the analyzers are ready for patient testing, we perform analysis on the samples, ensuring that the patient's results are consistent with their condition and no errors are found. Between our inpatient and outpatient centers, we run thousands of samples every day, prioritizing and juggling many tasks at once while producing accurate results.” “Right when we get in, we are putting samples on the analyzers, reading results and calling critical alerts or recollects,” added Rosalina Lunsford, Medical Lab Scientist. “Our chemistry analyzers have all the analytes one can think of. Each individual chemistry test that the hospital uses is calibrated, quality checked and reviewed by our chemistry maintenance experts.” Although there are many moving pieces when it comes to the work of our Core Lab experts, these team members work like a well-oiled machine in order to keep patient care at Renown Regional running efficiently. “I start my shift by reviewing my pending worklist and verifying any outstanding STAT tests; then, I track all my untracked samples for easy retrieval, and I'll go through my pending worklist again to make sure that everything is on track for proper turn-around time,” said Lindsey Randle, Medical Lab Scientist. "I'll retrieve anything that may need further special testing, and before releasing results, I will check the sample for any interferences or contamination. This process is on a constant loop throughout my shift in addition to performing analyzer maintenance and quality control testing at timed intervals. This is all done to ensure that we are releasing precise and accurate test results so that patients can receive proper treatment.” “We play a major role in keeping the hospital functioning,” added Rosalina Lunsford. “While the hospital doesn’t see us, we keep patient care moving. Core Lab is not stagnant; it is evolving each day. Tests are being added, machines are being updated and policies are changing. We see hundreds of patient results from different departments throughout the hospital. We analyze, question and conclude many times throughout the day and night.” Think of discovering a diagnosis and monitoring a condition as an ongoing investigation. Our Core Lab professionals are key detectives in the investigation, playing an essential – and often life-saving – role in the diagnosis, treatment and maintenance of each patient’s condition. “Oftentimes, we are the first to detect a patient's problem and escalate it to their provider,” said Lauren Anderson. “For example, looking under the microscope at a patient's white blood cells, Medical Lab Scientists may be the first to see a patient's leukemia and, with the collaboration of our pathologists, ensure that the next steps are taken towards diagnosis and treatment.
Read More About Department Spotlight: Core Laboratory at Renown Regional Medical Center
-
Renown Health Partnership with the Nevada Fitness Campaign
In 2021, Renown Health partnered with the National Fitness Campaign (NFC) to construct outdoor “Fitness Courts” in public spaces across the state. The partnership was formed to fight obesity, improve quality of life and create equitable access to outdoor exercise programs for communities around the state – bringing community wellness programs and free digital workouts to thousands of people. The Renown Health and NFC Campaign in Nevada is delivering outdoor wellness infrastructure to help communities stay active across the state and to change health outcomes. Out of Nevada's 16 counties, Fitness Courts® are now open in three. A Complete Bodyweight Workout at Seven Exercise Stations The Fitness Court is the world’s best outdoor gym that lets people use their own body weight to get a complete workout using seven exercise stations. Created for people ages 14 and over and with all abilities in mind, the workouts are adaptable for all fitness levels, allowing participants to move at their own pace. Users may also download the free Fitness Court App, which acts as a coach-in-your-pocket and enhances the outdoor gym into a digitally supported wellness experience. "Proximity to exercise opportunities, such as parks and recreation facilities, has been linked to an increase in physical activity among residents,” said Dr. Brian Erling, President & CEO of Renown Health. “Regular physical activity has a wide array of health benefits including weight control, muscle and bone strengthening, improved mental health and mood, and improved life expectancy. We are proud to bring additional access to exercise opportunities – at no charge, to everyone in our community.” Renown-Sponsored Fitness Courts Across Northern Nevada Rancho San Rafael 1595 N Sierra Street, Reno, NV 89503 South Valleys Regional Park 15650 Wedge Parkway, Reno, NV 89511 Ardmore Park 1200 12th Street, Sparks, NV 89431 Angel Park W Sage Street, Elko, NV 89801 Elquist Park 561 Altenburg Ave., Battle Mountain, NV 89820 To learn more visit Nevada Fitness Courts.
Read More About Renown Health Partnership with the Nevada Fitness Campaign
-
Do Mammograms Hurt? 4 Myths Debunked
Mammograms are an effective means for early detection of breast cancer. Still, many women shy away from them for fear of pain or discomfort. Let us debunk a few mammogram myths that will remove your worries and encourage proactive breast health. Reviewed by Dr. Colleen O'Kelly-Priddy, MD, FACS, breast surgical oncologist at Renown Women's Health. Myth 1: Mammograms Are Painful Reality: Although some women experience discomfort during a mammogram, most say it is not painful. Breast compression, which is important to get a clear image, can cause a sensation of pressure, but this lasts for a few seconds. Let your technician know how much pressure you can handle so you're not uncomfortable. Myth 2: Discomfort Persists Long After the Procedure Reality: The sensation of pressure developed through the compression process diminishes quickly after the procedure. Most women go about their day afterward without experiencing any residual pain.