Search
Results for 'what is an'
Clear-
5 Tips for Healthy Aging
September is National Healthy Aging Month, which is described by Healthy Aging Magazine as a “month designed to focus national attention on the positive aspects of growing older.” What does healthy aging mean to you? If you're like most people, you're looking forward to removing the negative from your life – negative energy, thoughts, people and activities that don't contribute to your best life. While we remain focused on ridding ourselves of the negatives, we can forget about ways to strengthen the positive parts of our lives. Dr. Shruti Basho, a family medicine physician at Renown Health’s senior-focused medical group, provides us with five positive behaviors to focus on to improve happiness and life satisfaction. Healthy Aging in 5 Easy Steps Connect – Humans are naturally social creatures! Build connections with friends, family, colleagues and neighbors. Strong interpersonal connections help enrich your life with new experiences and opportunities. Having a support system to call upon in both times of need and times of celebration is priceless, especially as you age. Forming these bonds helps you stay healthier and happier well into your aging journey. Joining the Sterling Silver Club is a great place to meet more people in the community who want to live a healthy, fulfilled life just like you. Be Active – Regular exercise, particularly as you grow older, is vital to increase and maintain your endurance, strength and balance. But exercise doesn’t have to be a chore! Pick a physical activity that you enjoy – whether it be enjoying a nature walk, taking a power weightlifting class or anything in between. Being active will also help you build strong connections with others. If you need a workout buddy in your neighborhood, Nextdoor is a great resource to find people who live right around the block from you and may be looking for their next exercise partner. Take Notice – Curiosity and mindfulness can be an impactful motivator in positive cognition and behavior as you age. Like a child, see the wonder and beauty of the world. Notice the things around you – the weather, the landscape, the mood and the feelings of people. According to Harvard Medical School, changes in the aging brain "enable us to become better at detecting relationships between diverse sources of information, capturing the big picture, and understanding the global implications of specific issues.” By taking notice, it’s easier to learn to appreciate the things that matter. Keep Learning – Engaging with lifelong learning is one of the best ways to keep your mind active. Keep trying something new! Challenges keep you on your toes and increase your confidence and excitement in your day. Don’t know where to start? EPIC (Educational Programs Inspiring the Community) offers a diverse personal enrichment and professional development curriculum at Truckee Meadows Community College ranging from art classes to accelerated training certificate courses. Give – Be generous with your time, your knowledge and your talents by giving to friends, family and the community when you have the capacity. Lending yourself to others doesn’t have to be taxing – saying thank you and even just giving someone a smile can change the course of someone’s day. If you’re looking for a hands-on way to give back, Nevada Volunteers is a great place to find volunteer opportunities near you. Renown Health is also always looking for volunteers who are passionate about making an unforgettable difference to the people and communities we serve. Practice these five tips to improve happiness and quality of life at any age.
-
Excellence in Heart Care Changes a Patient's Life
Being diagnosed with a chronic heart condition like atrial fibrillation (A-fib) can shift the course of your entire life. Embracing heart medications and lifestyle changes become your norm, and thanks to advancements in medicine and medical technology, managing the condition can bring you to a new sense of normalcy. But what if a different option was possible – one that would make medications and activity limits a thing of the past? This became the reality for Renown Health patient Richard Preyer after receiving a hybrid catheter ablation. Thanks to the vigilant surgical care of Shining Sun, MD, a cardiologist at the Renown Institute for Heart & Vascular Health, and his compassionate team, Richard has a new lease on life. Minimally Invasive with Maximal Results An A-fib patient since 2010 who had been living with an unfinished ablation, the 59-year-old Carson City resident turned to the internet to look for alternate solutions. He had heard that the Renown Institute for Heart & Vascular Health was a top-tier location for cardiovascular care. “I changed health insurance plans through Nevada Health Link to ensure I could see a Renown cardiologist,” said Richard. Choosing a cardiologist was an even easier decision for Richard. Dr. Sun’s introductory Find a Doctor video on Renown’s YouTube channel, where he displayed his expertise and determination, was more than enough for Richard to choose him as his cardiac care leader. At his first visit, Dr. Sun reviewed Richard’s records, and noted his prior unfinished ablation. The nine-hour procedure had been performed several years ago. With the enhanced technologies at Dr. Sun's disposal, Richard was excited at the thought of his life potentially being changed for good – with a minimally-invasive solution. Dr. Sun collaborated closely with Richard’s previous and current care teams – including a surgeon who performed a maze operation on him right before his surgery at Renown, to ensure his hybrid ablation was tailored uniquely to him. “Dr. Sun is clearly a very powerful cardiologist with many connections, and the coordination between his team and my other doctors was great,” said Richard. After working on the exterior of the heart in the first phase of the surgery and the interior of the heart during the second phase, Richard’s hybrid ablation was successful, completing the unfinished portion of his previous ablation. “Fixing A-fib can take one to three ablations, and sometimes it never holds,” said Richard. “That is one of the largest reasons why I am so thankful for this procedure and how it ended up.” Life After A-fib Now comes the long, arduous healing process, right? Not for Richard. With only eight incisions (four on each side of his chest), he was able to remove his bandages after two days, and he healed completely in one week. “I was even back to taking three-mile walks within a week of my operation,” said Richard. No more blood thinners. No more activity limits. And most importantly for Richard, no more heart-stabilizing medications that came with side effects he didn’t enjoy. He attributes his enhanced life to Dr. Sun and his team. “I highly recommend Dr. Sun and everyone that works with him,” he said. “Everyone in the group, from the nurses and anesthesiologists going above-and-beyond to the schedulers who helped me navigate the appointment process, made me have a lot of confidence. Their calm demeanors made so much difference.” Today, Richard now enjoys elongated walks in the northern Nevada outdoors, exotic vacations with his wife and, as he describes, “feeling like I’m in my 40’s again.” Learn more about the region's leader in cardiac health, heart and vascular care here.
Read More About Excellence in Heart Care Changes a Patient's Life
-
Three Emergency Room Options for You and Your Family
Renown Health has three emergency rooms open 24 hours a day, seven days a week, ready to serve our community. We checked in with Amy Hawkins, Manager of Clinical Nursing at Renown South Meadows, to learn more about the emergency room experience and how each can accommodate your emergency care needs. 1. Renown Regional Emergency Room The emergency room at Renown Regional Medical Center is the only Level II Trauma Center between Sacramento and Salt Lake City, treating more than 80,000 ER and trauma patients annually. Services Offered: This location offers immediate emergency care covered by general surgeons and coverage by the specialties of orthopedic surgery, neurosurgery, anesthesiology, emergency medicine, radiology and critical care. In addition, tertiary care needs include cardiac surgery, hemodialysis and microvascular surgery. (Patients may be referred to a Level I Trauma Center.) Renown Regional ER Location 2. Renown South Meadows Emergency Room South Reno is expanding, and so is Renown South Meadows ER! Exciting transformations are happening across this campus, including the new 121,000-square-foot specialty care center and upgrades to the existing medical center—expanding care to our patients. Added benefits to the more intimate setting at South Meadows: Smaller ER also means more personal experience. The team traditionally has more time to spend with each patient at the bedside. A smaller campus means convenient parking, as the ER is just outside the front entrance; however, patients are reminded to follow marked road signs when approaching the campus during construction. Most patients arrive by private vehicle versus an ambulance, so we are very accustomed to thinking quickly on our feet. Benefits to new construction: A new Cath lab will allow us to treat patients experiencing a heart attack and needing immediate intervention to open vessels in their hearts. Additional lab and imaging capabilities for our patients Services Offered: This location offers immediate emergency care staffed with board-certified emergency physicians. Patients can expect one-on-one interactions with trusted providers and shorter wait times. All emergency room services are open during construction, and patients are reminded to follow marked road signs when approaching the campus. South Meadows ER Location 3. Renown Children's Hospital Emergency Room This location offers immediate emergency care, with pediatric specialists always on staff. In addition, the Children's ER lobby is ideal for our littlest patients, with a child-friendly atmosphere and vibrant colors to help decrease the anxiety accompanying emergencies. Medical equipment is sized just for kids, and we offer a distraction machine, games and movies to help children cope with what can be a traumatic experience, like getting an IV. In addition, we have Child Life Specialists available to provide emotional support to both children and their families. When to Bring Your Child to the ER: Allergic reactions Asthma attacks Baby under three months old with a temperature higher than 100.4 degrees Fahrenheit Broken bones Burns Choking or poisoning Difficulty breathing Eye injuries Fainting, dizziness and confusion Head injuries Heart attack Rashes Seizures Severe bleeding Severe headache Severe pain Skin infections Stitches Stroke Venomous stings and bites Renown Children's Hospital Location
Read More About Three Emergency Room Options for You and Your Family
-
Understanding Your Risks for Fatty Liver Disease
Did you know that about one in four adults and one out of every ten kids in the U.S. might have a liver problem called non-alcoholic fatty liver disease (NAFLD)? This happens when too much fat builds up in the liver, and it's not because of drinking alcohol. The most serious type of this liver problem is called metabolic and non-alcoholic steatohepatitis (M/NASH). It means there's damage and can be scarring in the liver. About 20% of people with fatty liver disease have M/NASH. What's worrying is that many people don't even know they have it. Dr. Catherine McCarthy, a family medicine doctor at the University of Nevada, Reno School of Medicine, talks about the main risks of M/NASH and how you can check your risk for liver disease during Liver Health Matters Month, or anytime. Who Might Get M/NASH? Doctors aren't sure exactly why some people get fatty liver or M/NASH. While anyone can get M/NASH, people who might be more at risk include those with: Type 2 diabetes Insulin resistance or prediabetes High body mass index (BMI) or obesity High cholesterol or other fats in the blood High blood pressure Signs of liver problems from tests or biopsies A family member living with M/NASH How Do Doctors Find Out If You Have M/NASH? Doctors can do different checks and tests to see if someone has fatty liver or M/NASH. They might look at your liver health through non-invasive tests such as blood work, ultrasounds or MRIs. They might also suggest a special blood test called an Enhanced Liver Fibrosis (ELF) test– offered at no-cost through the Healthy Nevada Project – to check your risks of advancing liver disease. How Can You Treat Fatty Liver Disease or M/NASH? Patients with moderate to advanced liver scarring may also be prescribed a recently approved therapy called Rezdiffra. However, prevention of advancing disease is still the best option. Actions you can take to improve your liver health and reduce your risk include: Eating healthy, especially low-carb foods Exercising regularly Losing weight if needed Not drinking alcohol Keeping an eye on blood sugar if you have diabetes No-Cost Liver Screening Through the Healthy Nevada Project If you live in Nevada and are 18 or older, you can qualify for a no-cost liver health screening by enrolling in the Healthy Nevada Project, one of the largest community-based population health studies in the entire country. This study helps doctors understand your liver health better and plan early treatments to stop liver disease from getting worse. By joining the Healthy Nevada Project, you can: Get the FDA-approved ELF test to check your risks for liver disease See your test results in your medical record to help your doctor plan your care better Help doctors and researchers learn more about M/NASH and work on future treatments Participate in genetic sequencing for high-risk conditions linked to heart disease and certain cancers, including breast and ovarian cancer Gain high-level health insights, including food sensitivities, and ancestry information. Enrolling in the study is easy: Schedule a Virtual Consent Appointment through MyChart where a study representative will answer any questions, confirm your eligibility and sign you up. Once you’re signed up, your representative will schedule your blood test. Go to your blood draw appointment. By taking part in this study, you're helping to make a difference in liver health research!
Read More About Understanding Your Risks for Fatty Liver Disease
-
Book Ahead to Make Urgent Care More Convenient
How do you take the waiting game out of your Urgent Care visit? Book ahead! Here’s how this convenient service can help you schedule your appointment and see updated wait times at area urgent care facilities. We’ve all been there, done that: It’s after hours, you need to see a doc, and urgent care is slammed. Renown now offers a convenient option that will enhance your experience. Here’s How Book Ahead Works: From your phone or computer, you can check urgent care wait times around our region. This lets you see if the urgent care by your office is busier than the one closest to home — which may help your planning. Through Book Ahead, you can join the line at a specific urgent care just as you would in person. This allows you to stay home or at work as long as possible so you are more comfortable. Book Ahead When and Where to Receive Care We have many choices when it comes to our medical care. Should you visit a doctor’s office, urgent care, emergency care or make a Virtual Visit? It’s important to know which choice is right for your situation or condition. We asked Luis Palacio, M.D., with Renown Urgent Care to explain the differences and how to make your visit as smooth as possible. If you have been experiencing flu-like symptoms for less than 48 hours, call your doctor’s office. They can then determine if you can be treated with a prescription antiviral medicine. Visit urgent care or the emergency room only if you are unable to eat or drink anything and may be dehydrated, have a fever over 102.5 degrees F, or are experiencing shortness of breath. You can use Renown’s Virtual Visits videoconference service for flu-like symptoms so that you don’t need to leave the comfort of your home and you reduce the risk of spreading the virus to others. Virtual Visits allow you to see an urgent care provider from your home or office using a cellphone, computer or tablet with video capabilities. It is open from 8 a.m. to 6 p.m. Monday through Friday, and 9 a.m. to 4 p.m. Saturday and Sunday. How Do You Book Virtual Visits? Go to Virtual Visits to get started. Here, you’ll learn what virtual check-in is all about: It allows you to stay where you are and receive text notifications once a care provider is almost ready to see you. Click, join a line, and we will ask you some questions about your symptoms. This allows us to make sure you don’t need to call 911 or go to the ER. Reasons to visit the ER include stroke, chest pain, severe shortness of breath, uncontrolled bleeding, seizures and severe allergic reaction. If you answer “no,” you will see the wait times for each urgent care location. If you need to get in right away, you can select the location with the shortest wait time. Or, if time is not an issue and you’d prefer to stay closer to your home or office, you can select that location. Once you’ve selected a location, you input your cell number, name and number of patients. As your appointment gets closer, urgent care will text you with updates on timing. When you get the text message, you can choose to get “more time” and have your appointment pushed back, or tell them you’re ready to be seen and on your way. Learn more about how to Book Ahead at Renown urgent care below.
Read More About Book Ahead to Make Urgent Care More Convenient
-
Woman With Family History of Cancer Taking Action Today
With a family history of breast and other cancer, Aime′ Landaburu isn’t missing a single health screening. She recently had her first mammogram as well as a whole breast ultrasound, which detects 41 percent more cancers and reduces the number of false-positive results. Like many people, Aime′ Landaburu is busy juggling parenthood and a career. It would be easy to put health screenings on the back burner, but with a grandmother who has survived breast cancer three times and a grandmother who had ovarian cancer, Landaburu is addressing her family health history head-on. “I decided at 35 that I needed to get my screenings done because I have my family history of both grandmothers having had cancer,” Landaburu says. “In addition to the mammogram, I was really interested in doing the whole breast ultrasound. It is the same price as getting my hair done and it’s potentially something that could save my life.” Landaburu says the procedures were painless. “It was really comfortable, and the techs were all so nice and kind and gentle and explained things along the way.” Breast Screening Technology Provides Greater Insight George Krakora, MD, lead radiologist for Renown’s Breast Health Center, says the new 3D imaging for mammograms is picking up subtle cancers that would not have been seen with the previous 2D imaging. “It’s an additional tool that helps find those subtle cancers that may be missed in dense breasts,” Dr. Krakora says. With the whole breast ultrasound, the tech screens for masses — which are often obscured on the mammogram X-ray. Studies show it detects an additional 2 to 3 cancers per 1,000 women that would not have been detected with routine mammography. “Aime′ was noted to have heterogeneous dense breast tissue. That puts her at a little higher risk for cancer and also limits the sensitivity of mammography,” Dr. Krakora says. Multiple Ways to Screen for Breast Cancer However, Dr. Krakora notes, breast ultrasound is not a substitute for mammography, which can detect calcifications that can represent the earliest forms of cancer.” Surprisingly to Landaburu, her results came in just three days. “It’s so important to know what’s going on in your body. I was really nervous when I first got the paperwork, but ultimately it was negative, “ Landaburu says. “I’m thankful it was good and I have a baseline for the future.” Landaburu also advises other young women with a history of breast cancer to proactively communicate. She says it’s important to reach out to women they know who have survived breast cancer. “You have to take the first step and you want to be around for your kids and your family and yourself,” she says. “So utilize your resources, educate yourself and go get screened.” Breast Cancer Screening and Prevention Breast cancer begins when abnormal cells in the breast grow out of control. These cells form tumors that can grow into the surrounding tissue and spread to other parts of the body. Breast cancer occurs mostly in women, but men can also develop breast cancer. To schedule a mammogram or whole breast ultrasound, call 775-982-8100, or schedule an appointment online. Make an Appointment
Read More About Woman With Family History of Cancer Taking Action Today
-
Department Spotlight Clinical Research
May 20 is National Clinical Trials Day. Celebrate with us by recognizing the Clinical Research team at Renown Health! The root of every medication, treatment and procedure in healthcare can be traced back to research. From the beginning of the history of medicine, research has always played a crucial role in improving the lives of patients around the world, leaving a permanent mark on how we expand our medical capabilities to this day. Renown Health’s Clinical Research team, in partnership with the University of Nevada, Reno School of Medicine (UNR Med), are leading that effort in our very own community. As our in-house leaders of clinical trials, this team is dedicated to advancing the science of medicine to help further our bottom line of making a genuine difference in the health and well-being of the patients they serve. Trial by (Medical) Jury Every day looks different for the Clinical Research team, especially when it comes to interacting with patients, providers and “sponsors,” which are the organizations providing the treatment for the study. One fact always remains true: communication and collaboration are key, especially among the team who act as the face of this process. Meet Lisa English (pictured above on the far right in a blue shirt), a Lead Clinical Research Coordinator at Renown who serves as the study "project manager." One aspect of Lisa’s day-to-day is seeing patients through their clinical trials from start to finish. It all begins with the setup. “Before we can launch a study, there is a lot of back-and-forth dialogue between everyone involved to ensure the best fit,” said Lisa. “Sponsors will come to us with novel treatments, such as medications or devices, and the inclusion criteria that patients need to meet in order to qualify for the study. We then immediately jump into working with the providers, looking closely at the science and comparing the treatments to what is on the market already.” From there, Lisa coordinates conversations between the providers, sponsors and study teams to gauge everyone’s capacity based on the length of the study, ensuring everyone involved has the time to dedicate to the process. Next, the providers identify patients that meet the criteria for the study, and together, the team decides where the patient visits will happen and discusses any potential barriers that may affect patient retention. The budget is clearly defined at this stage, set up to make sure no patient is ever billed for medical costs incurred as a result of the study. Often, research participants are seen within the specialty clinics throughout the health system, while other times the Clinical Research Coordinators see patients at the recently centralized Clinical Research Office at Renown Regional Medical Center. This location provides an essential public-facing space for the community to learn more about clinical trials and demonstrates the breadth of resources available at Renown to sponsors to strengthen external partnerships and research funding opportunities. Once the study officially begins, team members like Lisa will set patients up for a “screening/qualifying visit.” During this appointment, she makes sure patients get scheduled for their lab work, imaging scans and anything else the provider may need to make an executive decision on whether or not the patient is a good candidate for the study. “I build it all in Epic,” said Lisa. “The study information, directions, requirements and next steps are all loaded in Epic for easy tracking. We are also required to input any notes in the sponsor’s electronic data capture website. All the information I track is inputted without protected health information (PHI), so every patient is completely anonymous.” After the patient officially qualifies, the study goes full steam ahead. Team members like Lisa and the providers receive continual updates from sponsors on the status of the study. “Throughout the entire process, I make sure patients get scheduled for everything that meets the requirements for the study,” said Lisa. “I meet with patients one-on-one to discuss their needs and concerns and ask questions about the study, organize their appointments and charts and deal with any issues or pivots that may arise. It’s very important that every patient fully understands what is going to happen with their care.” The Clinical Research department strives to serve as a care partner to patients, providers and clinics they work with. The majority of our Clinical Research Coordinators are trained phlebotomists and medical assistants, performing their own assessments such as lab draws and electrocardiograms (ECGs) to streamline the research visit process and reduce resource constraints on the clinics and health system. Lisa typically sees a couple of patients per week, depending on the study and where patients are in the cycle. Depending on the complexity of the trial, patients may see the research team only one time or several times over many years. Typically, clinical trial patients are seen in clinic every 2-4 weeks. There are many tasks required before, during and after a research visit to ensure everything runs smoothly, so Clinical Research Coordinators dedicate an average of 5-11 hours of work per patient, per visit. Regardless of patient load, each employee in the Clinical Research department – as well as participating teams across Renown and UNR Med – always step in to help each other out. According to Lisa, the environment is immensely supportive. “We have a program here at Renown to train employees who have never done clinical trials,” said Lisa. “We love seeing people get more engaged with the important work we do, and every department has been great at collaborating with us. Everyone brings a different perspective.” At the end of the study, Lisa gathers all the information and collects notes into a zip drive or paper binder for archiving. The sponsor lets the Clinical Research team, providers and patients know whether they are on the trial drug or on the placebo. The teams use the data gathered during the study to publish a report or present at conferences, promoting the critical research done to better the lives of patients in our community, and potentially, the world. “I appreciate the time everyone gives us to make sure our research is successful,” said Lisa. “It feels great to work together to make a difference, improve healthcare quality and save lives.” Behind-the-Scenes, Yet on the Frontlines The impact of research studies transcends hospital walls, and this can all be attributed to the dedication of our Clinical Research department. The constant collaboration between this team, lab science, medical assistants and providers, cardiology technologists, sonographers, finance teams and our partners at UNR Med is crucial to safeguarding the success of the studies. Devoted to keeping research close to home, Renown and UNR Med teamed up to form the Clinical Research Office (CRO) in 2021. With the strength of northern Nevada's largest not-for-profit health system and Nevada’s first medical school, this team is dedicated to giving our community access to the latest care innovations. “At UNR Med, we are working with students, residents and academic faculty; on the Renown side, we are working with clinicians and community participants,” said Amber Emerson, Manager for Community Outreach and Research Engagement for UNR Med. “Everything we do is data-driven,” added Kristen Gurnea, Manager of Clinical Research for Renown. “Our main goal is to optimize our impact and provide a community benefit for our patients. The scope of our roles in the Clinical Research office is very diverse.” To help meet the growing need locally for healthcare and cutting-edge treatment solutions, the CRO has continued to grow, expanding its research capabilities and helping bring new medications, medical devices and more to patients across northern Nevada and northeastern California. “Once upon a time, our team had only six members; today we have grown to a team of 25,” added Diana Torres, Research Resource Analyst for Renown. “We used to be considered one department, including Medical Education, and we have since branched off into our own cost center. We branched off even further and created a separate Genetics department that runs the Healthy Nevada Project. Throughout this process, the Clinical Research department was always the main point of the umbrella.” “We participate in hospital-wide outreach and marketing, and we feel this has really helped us get the word out about our department,” added Raul Arellano, Research Resource Analyst for Renown. “In fact, we doubled our clinical trial portfolio from last year.” The CRO currently operates over 100 clinical trials locally in cardiology, endocrinology, infectious disease, neurology, pediatric and adult oncology, pediatric sub-specialties and pulmonology. Behind the curtains of in-person research, the CRO is home to several experts who help turn our research studies into a reality, from budgeting and billing to barrier-breaking and building relationships. “I help with barriers patients and Clinical Research Coordinators are facing, building connections and relationships inside and outside of our health system,” said Kristen Gurnea. “I enjoy handling all the supporting pieces that are required for studies to happen.” “My role changes every day,” added Jenna Berger, Administrative Assistant for the CRO at Renown. “Some days, I’ll be helping coordinate patient stipends and going through document management to ensure we have all necessary signatures. Other days, I will be planning events – like Clinical Trials Week – for our department and creating marketing materials and fliers.” “Our day-to-day involves going over anything related to research financials,” added Diana Torres. “We handle sponsor billings, process efficiency and collecting revenue for research contracts, and we collaborate closely with our Finance department and Revenue Integrity in order to accomplish this. It’s important for us to make sure all billing on both the sponsor and patient side is taken care of, especially because patients should never receive a bill for medical services they receive for the trial. A year and a half ago, we started doing budget negotiations for research contracts,” said Diana Torres. “We are proud to help clinical teams with any training they may need on these negotiations as well as billing reviews and allocations.” Seeing patients progress during a study and transform before their eyes inspires the CRO team to continue doing what they do every day. “I’ve been here for many years, first working on the floor as an oncology nurse and transitioning to oncology research in 2005,” said Anna Winchell, Cancer Protocol Nurse for Renown. “I love getting to know the patients and seeing them progress into a healthy lifestyle.” Medical students and residents at UNR Med also play a significant role in the research process, advancing medicine by exploring causes and novel treatments for a wide range of conditions, including HIV, muscular dystrophy, gastrointestinal disorders, infectious diseases and more. Medical research at UNR Med is headed by committed research coordinators, community outreach managers, grants managers, pharmacists and physicians. “I oversee scientific review and help the physicians that come to us for those resources,” said Amil Trujillo-King, Medical Research Coordinator at UNR Med. “I guide medical students in their research protocols and help with different projects to improve research activities for both students and medical residents.” It takes a village to make clinical research happen. Because of that, the ACRO cannot thank the following teams enough for moving mountains for the future of medicine: Renown Health and UNR Med leadership for demonstrating the integrated health system’s commitment to expanding access to clinical research in our community within both the Renown / UNR Med affiliation and Renown active strategic plans. Renown Pharmacy especially Research Clinical Pharmacist Tim Morton, who supports all clinical trial medication dispensing and patient education across all clinical trials at Renown. Accounts Payable for having a huge impact on patient and employee reimbursement. Renown Medical Group for their participating providers, especially in oncology, cardiology, pulmonology, pediatrics, endocrinology and neurology, who are involved in research year after year. Marketing and Communications for helping with printed materials and raising awareness for clinical research at Renown and UNR Med. An Affiliation to Last Through the Ages A collective, shared vision of exploring community health – that is the impetus behind the affiliation between Renown and UNR Med. By leveraging resources across both institutions, the CRO has maximized their impact, giving the people of northern Nevada greater access to new interventions and treatments and promoting an impassioned culture with patients, providers, residents and medical students. “Community-based research always sat well with me,” said Amber Emerson. “As Renown and UNR Med, we have this unique opportunity to shape clinical research here in northern Nevada. We always make sure we present research in a meaningful way that speaks to the work we produce and demonstrates the opportunities we offer. After all, participating in clinical research doesn’t mean our patients are ‘guinea pigs’ – quite the opposite! They are partners in their health care, and we support them through providing access to novel treatments.” “Research is my passion, and my career has spanned broadly from grants administration to study coordination,” added Valerie Smith, Clinical Research Center Administrative Manager at UNR Med. “I am excited to be at the forefront of research frontiers in northern Nevada.” Through robust engagement and collaboration with healthcare providers, department administrators, internal research team members and leadership, the strength of this affiliation is unmeasurable. The CRO’s ultimate goal is to have clinical trials be the standard of care for every condition that Renown and UNR Med treats. Clinical research participation is all about patient autonomy, shared decision-making between patients and their providers and advancing medicine to save lives. From their beginnings as a small group of passionate researchers to their present reality as a leader in the research space in northern Nevada, their efforts do not go unnoticed. “The success of our department is inspiring,” said Amil Trujillo-King. “Renown and UNR Med supports the wellbeing of all employees and contributes directly to the growth of the department.” “When I first joined Renown in Patient Access, I didn’t realize that we had a research department; with a strong healthcare background in my family, I knew I wanted to grow in my career, and our expanding Clinical Research office was that next step,” said Raul Arellano. “With our affiliation with UNR Med, it’s especially inspiring to be able to apply what I learned as a Patient Access Representative to help further outcomes for our patients through managing our finances.” Through their unwavering commitment to research excellence and patient-centered care, the CRO will continue to pave the way for groundbreaking medical discoveries and improved outcomes for patients for years to come. “Fundamentally, we’re working to build a culture of research in our community because we believe it is the right thing to do. Our community deserves to have access to clinical trials and novel care close to home with a dedicated team to support them every step of the way,” closes Kristen Gurnea.
-
Department Spotlight: Wound Care
For the average person, wounds aren’t an everyday worry. However, for at least eight million Americans, chronic wounds can pose a serious threat to health and well-being. From a person with diabetes experiencing painful neuropathy to a patient healing from a significant burn, caring for advanced wounds is a major part of their healthcare journey. Who do they go to get the care and guidance they need? The answer: Renown Wound Care. Serving patients in both the inpatient and outpatient settings, this department provides comprehensive, best-in-class treatments for severe and chronic wound healing and ostomy care. Our Wound Care team members have mastered the art of harnessing cutting-edge technologies and a patient-centric approach to redefine the standards of healing. Advanced Care for the Best Repair At Renown Health, we are fortunate to have a team full of nurses, physicians and more caring for patients with wounds caused by a wide variety of conditions. Those include: Burns Trauma Vascular diseases Radiation therapy Pressure ulcers Diabetes and diabetic neuropathy Adding to the expert-level continuum of care, Renown is the only health system offering complete ostomy services in the entire region. The Wound Care team helps ostomy patients with the fitting of their medical bags, treatment of any skin conditions that may arise after ostomy bag placement, care coordination and much more. With a multidisciplinary network of experts tailoring personalized treatment plans, there is never a dull moment on the floor. On the outpatient side, the team expects 50-60 patients in one day alone. “As a clinician, wound care is a lot of ‘arts and crafts,’ so we get to use our creative and critical thinking skills to provide the best possible care,” said Samantha Moore, Advanced Wound Care Specialist RN for Outpatient Wound Care. “Each patient has an individualized plan of care – we greet them as they come into the clinic, escort them back to their treatment rooms and get their latest health updates and life situations before providing wound or ostomy care. We prepare each morning doing chart reviews to determine patient needs, wound progression and referral needs.” “We are a highly specialized, dedicated group of professionals with a passion to treat and heal our patients’ wounds,” added Lori Conner, Advanced Wound Care Specialist RN for Outpatient Wound Care. “When a patient comes to our clinic for evaluation, they are given a dedicated appointment to thoroughly go over their medical and surgical history, medications and nature of the wound.” Switching over to the inpatient care team, they operate like a well-oiled assembly line, navigating different daily assignments with precision and flexibility. “On the inpatient side, our day starts in our office with triaging our consult list; after the triage process is completed, we get our assignments, which can consist of wound vacuum-assisted closure (VAC) patients, follow-up patients, ostomy education patients and new wound consults,” said Megan Uy, Advanced Wound Care Specialist RN for Inpatient Wound Care. “In the case of patients requiring wound VAC changes, we consider what kind of pre-medication for pain that they need. Although some patients may be seen on a time schedule, the day ends up flexible as patients are being seen by other specialties. This flexibility also benefits the patients, making them feel more empowered with their care.” “Each day in the inpatient setting, we get to our office and sort through all the new consults that came in overnight, and the charge nurse makes the assignment for the day,” added Madison Arlin, Advanced Wound Care Specialist RN for Inpatient Wound Care. “After the assignment is completed, each nurse is responsible for researching their patients and organizing their day, typically by priority – wound VACs and ostomies usually take top priority.” Now, how do these treatments actually work? This specialized field handles advanced methods of treating each condition, including: Biological skin substitutes Surgical debridement Advanced wound dressings Negative pressure therapy Pre-ostomy markings and education Offloading techniques, such as padding or dressing “Before starting treatments, we communicate with our nurses and providers to make sure that the patient is comfortable prior to wound care,” said Dianna Seo, Advanced Wound Care Specialist RN for Inpatient Wound Care. “After we see the patient, if there is a need for escalated care, we contact the provider for additional testing or consults. We continue to follow-up on patients that have severe wounds, wound VACs and ostomies.” In the hands of the Wound Care team, patients exit our hospital walls not only restored but also empowered, set on a trajectory for long-term healing. Your Expert Care Guides No matter the case or the severity of the wound or condition, patient care, comfort and communication always come first – before, during and after treatment. “Many of our patients have chronic needs, so we end up seeing them for several months, if not years in some cases; we stay up to date with their specific psychosocial needs and help remove barriers that would prevent their wounds from healing,” said Samantha Moore. “I enjoy knowing that my positive attitude can improve our patients’ days,” added Maddie Pauley, Patient Access Representative for Outpatient Wound Care. “When they’re routinely coming to appointments they might not enjoy, hearing them praise our team and give their thanks is one of the most rewarding feelings.” As a wound care patient, there can be a lot of unknowns when beginning their care journey. However, these team members carefully walk each patient through every step from beginning to end. “When we go to see a wound care patient, our team is very consistent about explaining to the patients what our role is and what we plan to do with their wound, and then we continue to actively communicate throughout wound care each step that we are doing as we are doing it,” said Madison Arlin. “We also encourage some of our patients to listen to music that they enjoy during the wound care, or we will cover their eyes with a cloth if they request so that they don't have to see their wound. Sometimes, we will ask the family to stay at the bedside to hold their family member's hand.” Education is crucial to ensuring each patient knows what to expect in order to care for their wound and understanding the stages of healing. Fortunately, this team is well-versed in the world of wound wisdom. “A lot of education is provided on the type of dressing we are applying, and if the patient is going to be performing their own dressing changes, we will go over the entire change with them and provide supplies for discharge,” said Megan Uy. “Additionally, there will be written instructions in their discharge paperwork. In the cases of wound VAC dressing changes, each step is explained to the patient before doing it, and we also go over discharge options and expectations.” “As a clinician who sees a lot of patients prior to having their ostomy placed (pre-surgical marking), one of the most important things we do is first sit with the patient and/or caregivers and talk about their fears, concerns, questions and goals,” said Samantha Moore. “We provide a lot of emotional support and education, helping identify community resources. For our wound patients, we spend a lot of time educating our patients/caregivers about how and why their wounds occurred. We try to connect with them on a personal level and help them identify ways to help their wounds heal.” To see a patient’s care journey from the second they enter through our doors to the moment they return home is one of the most rewarding feelings for the Wound Care teams. In fact, they’ve had the pleasure of treating patients for years and seeing their wounds almost completely heal. The team collectively values the successful healing journeys of their patients as their proudest achievement. “One of our team's greatest accomplishments was being able to see one of our long-term patients discharged with nearly resolved wounds,” said Megan Uy. “This patient had been in our care on-and-off for the past year with many hospitalizations and had complicated high-output enterocutaneous fistulas within his wound bed. These were incredibly hard to keep a dressing on successfully, and he often had issues with the dressing leaking. Eventually, we got a dressing that could remain intact until his next scheduled dressing change, and he was able to get surgery that fixed his fistulas. Being able to see him recover and heal his wounds was a very large accomplishment for us.” The admiration and compassion this team has for their patients also extends to each other. The cohesive way they work together only further benefits their patients, offering the best-possible collaborative care. “We have extremely skilled clinicians in our group that are not only incredible in the work that they do and the patient care that they provide but are also enjoyable to work with as well,” said Geane Weaver, Advanced Wound Care Specialist RN for Inpatient Wound Care. “There is something to be admired in each and every one of my coworkers.” “Our team is very close and supportive of each other at all times,” added Madison Arlin. “I feel very lucky to work with such an amazing group of people. Our team is very proud of the work we do.” Fervently Fighting the Good Fight So, with the highly specialized nature of advanced wound care, how did these team members get inspired to join the Wound Care team in the first place? Well, for many of these devoted employees, their first exposure to caring for wounds took place on different units – sparking their interest in making wound care their full-time career. “Renown was the most welcoming towards me as a student nurse, and I liked that it was a teaching hospital,” said Madison Arlin. “I started in the General Surgical Unit (GSU) immediately after graduating nursing school and worked there for two years before transferring to wound care. I decided to apply to the wound team after watching the wound nurses do wound VACs and ostomy changes on the floor. I would ask them if I could watch, and I was always very fascinated by the wound healing process.” “Prior to joining the inpatient wound team, like Madison, I was also a bedside nurse in GSU,” added Geane Weaver. “Working on that floor, I was already exposed to a lot of patients that were requiring some kind of advanced wound care in one way or another. Working in the GSU, I also cared for a lot of patients that had wound VACs and ostomies. These patients make up a huge group of the individuals that our team sees on a regular basis, and they've always been intriguing for me, so naturally, wound care has always been on my radar.” For other team members, wound care has always been a point of curiosity throughout their education and career. From their very first exposure to this care area, they were hooked. “I was always curious about wound care even through my nursing school experience,” said Dianna Seo. “When I was working on the floor, I would trade to do wound care for patients. When I had time, I would follow wound care and help when I could. I joined the skin team which drove me to be increasingly involved with wound care. As soon as there was a job opening, I applied for the position. I worked in outpatient wound care for approximately four years and now inpatient for another four years. I have enjoyed all aspects of wound care and patient care.” “I had great clinical experience at Renown when I was in nursing school; I also was very interested in caring for trauma patients, and Renown being a Level II trauma center aligned with my interests,” added Megan Uy. “I began my nursing career in the GSU, but my dream job was always Wound Care. During my nursing school clinicals, I had the opportunity to watch some members of the wound team do wound VAC changes and thought it was incredibly intriguing and a great combination of utilizing the knowledge of anatomy and physiology while being creative with handicraft. A position opened on the team around the time I met the prerequisites to be eligible for the position, and luckily, I got it.” Our Wound Care team has achieved significant employee and departmental milestones over the past year, reflecting their dedication to enhancing patient care and overall process improvement. “We have had many accomplishments within the last year and are currently working on more to improve the hospital,” said Dianna Seo. “Madison Arlin won the DAISY Award for her great work with our patients. Megan Uy won Top Talent of the Quarter for helping a stranger. Ande Ferriera has worked tirelessly to improve our process improvement. Allie Saunders, as our leader, has worked to improve patient skin by getting new beds for Renown Regional. All our patients that have healed or are on their way to healing under our care is our greatest achievement that we as wound team is most proud of.” “We are constantly updating protocols, notes and orders for bedside nursing so that it is a more straightforward and seamless charting process,” added Madison Arlin. “We have representatives of different supply companies come and present new products that we think may benefit our patients better. Our wonderful tech has even updated our department site on Inside Renown so that the nurses always have references available.” Renown’s strong influence in the region – and the opportunity to give back to their community – was, and continues to be, a major draw for this team. “Since I can remember, Renown has always been the most prevalent healthcare name for my family and has always taken the most amazing, thorough care of my loved ones,” said Maddie Pauley. “I have always wanted to work somewhere I could help people, and starting at Renown has really opened my eyes into how much of a difference each one of us can make.” Our Wound Care department’s success stories and proactive approach not only reflect their passion for healing but also inspire a ripple effect of positive change throughout our health system. They proudly exemplify a shared commitment to enhancing the well-being of all patients under their care. “Being part of Renown and part of this team has been my blessing; I get to do a job I love with people that love it too,” closed Dianna Seo.
-
Most Common Reasons Women Visit the ER
If you or someone you know is experiencing a medical emergency, it's essential to seek immediate attention by calling 9-1-1 or visiting the ER for a thorough evaluation by a trained medical professional and timely intervention. Access to a convenient and trusted emergency room (ER) is critical to any person’s healthcare needs, including medical emergencies related to women’s health. We explored some common scenarios and warning signs prompting women to seek immediate medical attention with Aiden Gould, Board-Certified Emergency Physician at Renown Health. When your medical emergency can’t wait, Renown ER is here to provide you with the region’s leading emergency care to diagnose and treat your condition or illness. Understanding Common Reasons Women Visit the Emergency Room Gynecological Emergencies: One of the most common reasons women may seek emergency care is due to gynecological emergencies such as severe pelvic pain, abnormal bleeding or complications related to pregnancy. These issues can be alarming and warrant immediate medical attention if the issue persists or is out of the ordinary for you. Emotional and Physical Well-Being: For those facing diverse medical or mental health emergencies, seeking prompt assistance is crucial for a thorough assessment and safe, timely intervention. Renown ER teams are equipped with trained professionals who provide compassionate care for individuals seeking help in the following situations: Suicide risk assessment and intervention Substance abuse assessment Assault and trauma care Crisis support and intervention Resources for ongoing care and well-being support Severe Abdominal Pain: Unexplained and severe abdominal pain that is substantially different than what is normal for you is a symptom you should never ignore as it can indicate underlying issues. Warning signs of an acute medical situation include fever, vomiting or a rapid change in motor function and inability to move due to pain. Respiratory Distress: Difficulty breathing, persistent coughing and other respiratory issues can be especially concerning. Women with pre-existing respiratory conditions like asthma or those experiencing sudden respiratory distress should seek immediate care from a medical professional. Warning signs of respiratory distress may include a significant change in one’s breathing rate, changing of the skin color to blue, gray or paleness due to lack of oxygen, nose flaring and chest retractions. Cardiovascular Emergencies: Heart-related issues are not exclusive to men. Women can also experience cardiovascular emergencies that often go undiagnosed because symptoms differ from men. Symptoms like chest pain, extreme fatigue, vomiting or pain in the abdomen, shortness of breath or palpitations should be evaluated by an emergency medical professional as timely intervention is critical in such cases. Renown leads the region in cardiology care with our technological expertise and patient-centered approach. Our comprehensive team diagnoses heart disease and other cardiac conditions, offering personalized treatment plans. Neurological Symptoms: Sudden and severe headaches, seizures or other neurological symptoms may prompt women to visit the ER if symptoms are extremely disorientating or debilitating. These symptoms could be indicative of various conditions from mild to severe, including strokes or neurological disorders that require prompt evaluation. Renown Regional Medical Center is a Comprehensive Stroke Center, providing primary stroke care including evaluation, treatment and education to patients who arrive at a Renown facility with the signs and symptoms of a stroke. Compassionate Care in Times of Need At Renown Health, we understand that your time is valuable, especially in emergency situations. That's why we strive to provide patients with exceptional care, compassion and respect. Plan ahead and make informed decisions about seeking medical care by viewing your estimated triage wait time at a Renown ER.
-
Department Spotlight: Children’s Infusion Services
Help us celebrate the holiday season by sharing joy with our Children’s Infusion Services team! Thinking about blood can make any of us squeamish, and seeing it can be even more intimidating to the children in our lives. Being treated for a condition that requires blood transfusions or chemotherapy infusions is no easy feat, especially during the holiday season. This time of year, we are proud that we can offer our pediatric patients the power of proximity and excellence by having access to high level care close to home. The Children’s Infusion Services (CIS) department at Renown Children’s Hospital is committed to bringing the gift of quality care to our community’s youngest patients. Whether they are caring for a child with a blood disorder or giving expert infusion care for a child battling cancer, no team does what they do better than these expert nurses, medical assistants, intake coordinators and physicians. ‘Tis the Season to Bring Hope As the only pediatric oncology and hematology program in the region, the CIS department has a lot of responsibility on their shoulders. From inpatient chemotherapy to outpatient infusion services, this team treats a long list of pediatric blood conditions including: Pediatric cancers Anemias Immune-mediated blood disorders Sickle-cell disease Bone marrow failure syndromes Bleeding disorders “Our team provides a large variety of services from labs draws, sedations for procedures, infusions for diagnoses such as Crohn's disease, blood transfusions, as well as chemotherapy,” said Jen Torres, RN. “Our team works extremely well together. We try to go above and beyond for our patients every day. It may be something as simple as a hug to comfort a parent or a special birthday gift for a patient.” “My job allows me to work with several departments and providers when coordinating care for our littlest of patients,” added Jane Strawn, Intake Coordinator. “I assure proper authorizations are in place for the care that is needed, I communicate with our families when scheduling appointments, I organize End of Treatment Celebrations, as well as birthday shout outs and work closely with our Child Life team to help make the challenging appointment little easier.” To best serve their patients, the team thrives on being expert multitaskers. Central line care, chemotherapy administration, blood transfusions, medication management, preventative injections, lab draws, lumbar punctures, biopsies, imaging – you name it, they do it. And they do it all with the utmost focus on safety and support. “Our days have a lot of variation, as we perform a number of different services,” said Meagan Bertotti, RN. “We provide infusions for patients with chronic or acute medical conditions and chemotherapy/biotherapy treatment to patients undergoing cancer treatments. Overall, though, we work as a team to make these difficult procedures and treatments as easy as possible for the patients and families by providing engagement and support.” “While we handle a lot of chemotherapy treatments for pediatric patients, we also do other infusions and transfusions as well such as blood and platelet transfusions, enzyme replacement therapies, different types of injections such as Rabies vaccine or Synagis for high-risk babies who need that extra protection during the RSV season, and lab draws,” said Chelsea Angues, RN. “We care for patients that get their therapies from outside hospitals, but the patient lives within the Reno area. We receive orders from those outside hospitals to care for those patients, so they can still be with their families and not have to travel.” As members of the Children’s Oncology Group, a highly-regarded clinical trials group where over 90% of pediatric cancer patients across the U.S. receive treatment, teams like CIS in Renown Children’s Hospital deliver the highest standard of care. This partnership is a true testament to the devoted collaboration and relationship-building this team commits to on behalf of their patients every day. "One of the biggest accomplishments of our team is the fact that we became a member of the Children’s Oncology Group, and the Children's Infusion Center and Pediatric Oncology became one unit,” said Shelby Nolte. "Instead of being a clinic on one side and an infusion center on the other, we really came together to make it a whole unit that collaborates on almost everything.” “We've put much time into trying to understand other departments, their flow, their rationales and their processes so we can come to a solution that benefits our patients the greatest,” added Tiffany Macie, RN. “We've taken the last few years to really build our relationships with our pharmacy staff, our lab staff and our central supply resources. Our relationship building extends beyond the walls of the Renown building as well and out to the community providers too. In the past few years, we've been able to build relationships with the providers in the community where they trust they can send us their patients for treatment and lab draws. Finally, we've spent much time working on the relationships as a team. It's emotional work we do on our unit, and these families become our family. It's important to us that we take the time to be together outside of our shifts to enjoy one another and laugh!” In the compassionate realm of pediatric healthcare, CIS knows that the complexities of a cancer or blood disorder diagnosis can take an emotional toll on their patients and families. The team firmly believes that emotional support can be as important as the physical and medical support throughout each patient’s unique care journey, striving to be a comforting presence during daunting times. “The most important part of my day is collaborating with the Children's Infusion team to make life manageable for the families that are going through this experience,” added Shelby Nolte, Senior Medical Assistant. “We work as a team to make life easier for the blow of a cancer diagnosis. We are there for our families in every way. If they need a shoulder to cry on, an ear to listen or just someone to play cards with or tell a funny story too, we are there.” “One of the things our team does extremely well to help our patients and their families with new diagnoses is to simply meet them where they are,” said Tiffany Macie. “That looks different for every family and every patient. We work in an environment where can build relationships with our patients and their families. This allows us the unique opportunity to really get to know them. We learn their fears, their joys, their worries, what their family lives are like, and we learn how to best meet them where they are.” Transcending the conventional boundaries of care, the CIS department closely supports each patient, offering them solace tailored to the unique fabric of each family's life.
Read More About Department Spotlight: Children’s Infusion Services
-
5 Benefits of Medicare Advantage Plans
If you are approaching age 65, you may be starting to think about the government benefits you will soon qualify for. For example, your healthcare option to elect between Original Medicare or a Medicare Advantage plan. What’s the difference? Original Medicare comes in two parts: Part A and Part B. Part A covers a portion of hospitalization expenses, and Part B applies to doctor visits and medical expenses, such as lab tests and some preventative screenings. A Medicare Advantage plan, also known as Part C, is an “all-in-one” alternative to Original Medicare. These “bundled” plans include the benefits of Part A, Part B and Part D (prescription drugs). Some people choose a Medicare Advantage Plans over Original Medicare because these plans offer coverage like vision, hearing, dental and more. Saves You Money First and foremost, Medicare Advantage Plans save Medicare members money –and not just a little bit of money, but a lot of money. Original Medicare only pays 80% of the cost of medical care – the Medicare beneficiary is responsible for the other 20%. A Medicare Advantage Plan is different. The Medicare Beneficiary is only responsible for a small copay, typically less than 20% of a doctor visit or procedure. More importantly, Medicare Advantage Plans have a maximum out-of-pocket amount, meaning that once you reach the limit, the Plan pays 100% of all medical services. That alone can save thousands of dollars per year – particularly if there is a hospitalization involved. Dental, Vision and Hearing Coverage What sets Medicare Advantage plans apart is the additional benefits provided that Original Medicare doesn’t cover. These benefits include dental coverage, vision coverage, hearing exams and hearing aid coverage. None of these important health care benefits are included in Original Medicare. Also, most Medicare Advantage Plans include prescription drug coverage at no additional cost, while individuals with Original Medicare need to sign-up and pay extra for Part D prescription drug coverage. Medicare Advantage Plans offer more benefits than Original Medicare and they help members save on their health care costs. Focus on Accessibility, Wellness and Preventative Health Accessible healthcare coverage is key to staying on top of your health. To join a Medicare Advantage Plan you must have Part A and Part B coverage and live in the plan’s service area. It is important to remember that Original Medicare is only valid in the United States. Fortunately, many Medicare Advantage Plans offer worldwide emergency coverage. Another important healthcare consideration to keep in mind is Medicare Advantage Plans focus on your overall well-being. They offer preventative and wellness-related benefits at no cost to you. This includes important benefits like free over-the-counter medicines and free gym memberships. You won’t find those types of benefits with Original Medicare. Medicare Supplement Plans (Medigap) Some people confuse a Medicare Supplement Plan, also known as a Medigap Plan, with Medicare Advantage Plans. They are different and the biggest difference is Medicare Supplement plans come with ever-increasing premiums because they are based on your age. This means the cost of these plans increase every year. Plus, they don’t offer any supplemental benefit coverage like vision, dental or hearing. That’s not the case with a Medicare Advantage Plan. In many cases, there is no monthly premium and you receive all manner of supplemental benefits. These benefit-rich, zero-dollar premium Medicare Advantage plans are enticing people to say goodbye to pricy Medicare supplement plans and hello to Medicare Advantage Plans. Don’t worry, if you join a Medicare Advantage Plan for the first time and you aren’t happy with the plan, you’ll have special rights under federal law to buy a Medigap policy and a Medicare drug plan if you return to Original Medicare within 12 months of joining the Medicare Advantage Plan. The Flexibility to Change Your Mind A common misconception about Medicare Advantage Plans is that when you join, you are still on Medicare and are not giving up your Medicare coverage. Medicare Advantage Plans are considered “Medicare Part C.” This means they combine your Medicare Part A (hospital coverage), Part B (doctor’s coverage) and Part D (prescription drug coverage) into one convenient package that costs less and provides more. You can only join, switch or drop a Medicare Advantage Plan during the enrollment periods: Initial Enrollment Period: When you first become eligible for Medicare, you can sign up during your Initial Enrollment Period. For many, this is the seven-month period that begins three months before the month you turn 65, includes the month you turn 65, and ends three months after the month you turn 65. General Enrollment Period: If you have Part A coverage and you get Part B for the first time during this period (between January 1 - March 31 each year), you can also join a Medicare Advantage Plan. Your coverage may not start until July 1. Annual Election Period: Between October 15 and December 7, anyone with Medicare can join, switch or drop a Medicare Advantage Plan. Your coverage will begin on January 1 (as long as the plan receives your request by December 7). Medicare Advantage Plans have been around for more than 25 years and continue to grow in popularity. In some parts of the country, more than half of all Medicare beneficiaries are enrolled in a Medicare Advantage Plan. Only 40% are enrolled here in Nevada, but that number is growing every year.
-
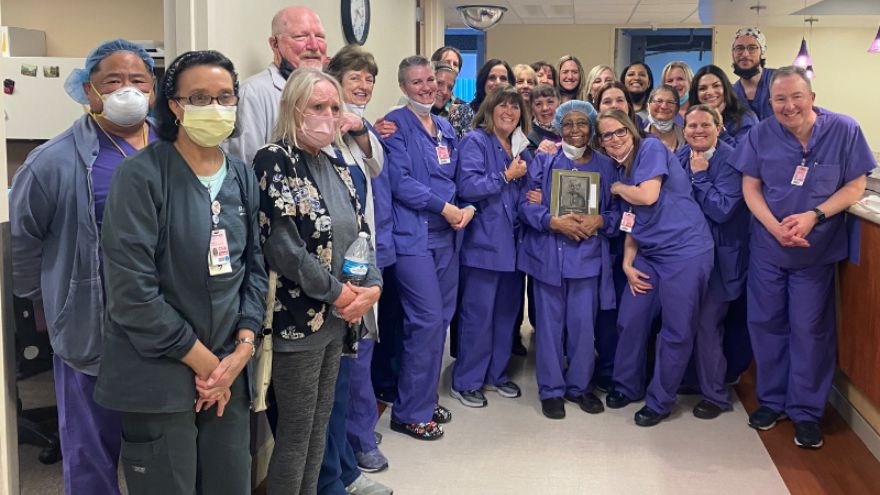
Department Spotlight: Labor & Delivery
Parents welcoming their new bundles of joy into the world might be overcome with emotions. They're exhausted yet excited to meet their new baby and hold them in their arms. That’s where Renown Health’s Labor & Delivery (L&D) department comes in. When patients arrive at the L&D unit in Renown Regional Medical Center, they are embraced with caring, compassionate nurses, surgical technicians and physicians ready to serve their family. As they get ready for the big moment in their private L&D room or family suite, you can be certain that you, they can be certain that they will receive the excellent care they deserve. Unpredictable, but Never Unprepared Ushering in new life can bring a lot of surprises for parents, but the L&D department is prepared for any challenge. Whether the unit is helping with a routine or high-risk delivery, every patient and newborn are treated with personalized care that is uniquely tailored to their own individual needs and birth preferences, from labor evaluation and birth to post-birth lactation consultation and navigating the nursery. “Our floor is never predictable,” said Bri Goode, Renown L&D nurse. “Our nurses and our staff work as a team to ensure the best care for our patients. I commonly say that we are all 'nurses’ for each patient!” The state-of-the-art technology at their fingertips – including advanced 3D ultrasound machines – coupled with the love and passion the team has for their patients allows them to create an optimal environment for every mother and baby. The unit is also equipped with a Labor Assessment Area, where expectant mothers are evaluated to determine what stage of labor they are in, removing the guesswork and allowing providers to treat the patient and unborn child more efficiently and meet them exactly where they are at in the labor process. Nothing can replace the careful guidance and words of encouragement a patient needs in the delivery room. The L&D department are true patient advocates and firmly believe in the power of listening and the power of staying calm and collected. “To help our patients and ease their fears and anxieties, we always ensure them that our biggest goal is to have a healthy mom and healthy baby,” said Lindsay Strowmatt, Renown L&D nurse. “We constantly reinforce that they are strong and capable. Empowerment goes a long way!” “We always take the time to actually sit down and listen to the patient, no matter how busy we are,” added Krystie Mortensen, Renown L&D nurse and DAISY Award winner. “It’s important for us to understand where their nerves are stemming from and address any changes in plan of care along the way.” While the L&D unit is seen as a “happy place,” as described repeatedly by the members of the team, a seemingly low-risk patient can also turn into an emergency in a matter of seconds. "Our line of work can involve high-stakes emergency care,” said April Tucker, Renown L&D nurse. “We view change as a necessary part of growth, and we save lives.” These steps result in high patient outcome scores, which can be attributed directly to the unit. “We have continually great outcomes from hard work and consistency in care,” said Roya Galata, Renown L&D nurse and Nursing Organizations Alliance (NOA) Lifetime Achievement awardee. “I have tremendous love for my patients and the type of work I do.” Awards Without End With patient safety and experience always top of mind, and with the team continually going above and beyond for all parents and their newborns, it’s no wonder why the L&D department has achieved a long and growing list of both local and national awards and accolades. This year, U.S. News & World Report ranked the L&D unit at Renown Regional as "High Performing in Maternity Care – Uncomplicated Pregnancy.” This award is only the latest in this department’s “Best Of” accolades list, as the unit also achieved a win as the Best Place to Have a Baby in the 2022 Best of Reno Awards. Not only is the department continually recognized, but individual team members also receive coveted awards within their professional associations. As previously mentioned, Krystie Mortensen is a DAISY Award winner, which means that she has been recognized for the “super-human work” she has done throughout her career. Additionally, three team members, including Roya Galata, have received NOA awards, celebrating their contributions to the nursing profession as a whole. Many nurses in this department also choose to pursue lifelong learning by taking advantage of the educational benefits that Renown offers. Several team members have completed their continuing education in midwifery and advanced practice, reaffirming their dedication to delivering healthy babies and helping parents manage their first few days with their newborns. “The teamwork on this unit is phenomenal, and the energy and commitment that the staff comes in with every single day amazes me,” said Lora Carlson, Renown L&D Manager of Nursing. Internally, the L&D department loves to show their spirit at Renown. In December, they received the Best Holiday Decoration award during the 2021 holiday season. The team also enjoys participating (and scoring well) in Renown-sponsored Halloween costume contests. In 2023, the L&D department will only pursue greater heights to continue producing patient outcomes. A Work Family “I stay here because this is my family. My work family.” These strong words were proudly stated by Jeanne Bufkin, Renown L&D Surgical Technician, and echoed by virtually every L&D employee. Having each other’s backs during both times of need and times of celebration is a must in this department, and they do so proudly. “Our staff constantly back each other up,” added Lora Carlson. “They display a lot of adaptability and flexibility. That’s why our unit functions as well as it does.” Several team members in this department experienced the care of the L&D unit at Renown before they became fully-fledged employees. “I had two of my babies here and had wonderful experiences both times,” said Judy McBride, Unit Clerk. “I love being a part of the reason why the next woman can say the same!” Bri Goode also delivered her child at Renown and loved her experience so much that she was also inspired to join the team. “I chose to work at Renown because when I had such a positive experience during my delivery while I was in nursing school, I knew it was a team I wanted to be a part of.” Coming to Renown was clearly an easy decision for this team; staying at Renown is even easier. “I stay here because I love what I do and who I do it with,” said Judy McBride. “I truly feel like I am treated as an asset to this department, and it makes me want to come to work every day and make a difference in these mothers’ lives.” The closeness of this department and the top-of-the-line collaboration displayed by every provider can be felt by the patients during their entire stay at Renown. “We have an amazing collaborative team of physicians, nurses, scrub techs, unit clerks, patient access representatives and environmental services personnel that strive to provide our patients with the best possible care,” said April Tucker. The labor and delivery process is a team effort – and those interested in jumping in on this team effort are welcome to join. Delivering healthy babies and supporting new mothers are cornerstone acts in meeting Renown’s mission of making a genuine difference in the communities we serve. Our L&D department does precisely this and more, never giving up in Fighting the Good Fight.






.png?rev=5ac90884d83d45468d7e3a5389920ff1)