Search
Results for 'doctor'
Clear-
Anesthesiologist - Carson Valley Health - Full Time, Beautiful Gardnerville, NV
Full Time - Eligible for Benefits510701 AdministrationVaries -
Women's Heart Center Cardiology Program Director
Full Time - Eligible for Benefits510701 AdministrationVaries -
 Greenberg Breast Health Center at Renown - VistaGreenberg Breast Health Center at Renown - VistaHours
Greenberg Breast Health Center at Renown - VistaGreenberg Breast Health Center at Renown - VistaHours
Mon-Fri7 a.m. - 3 p.m.Sat-SunClosed -
Make Hydration a Priority for Your Health
As the temperatures skyrocket and we return to more outdoor activity, one thing is certain: you must hydrate to stay cool, healthy, and functional. But how much water do you need, and what are some easy ways to ensure you are getting enough? Aurosis Reddy, DO a family medicine provider with Renown Medical Group, shares what you need to know. How Much Water Is Enough? Experts agree that recommended daily water intake can vary depending on different factors such as your weight, metabolism, location, diet, physical activity, and health. As a rule of thumb, women should aim for a daily fluid intake of 91 ounces, and men should aim for 125 ounces. It is important to listen to your body and recognize when you might need to increase your water intake. For example, if you’re partaking in strenuous exercise, or spending time outside in the heat, you’ll want to give your body more water and electrolytes to function properly. How Can I Tell If I Am Dehydrated? Decreased coordination Fatigue Less urination Dizziness Dry, sticky lips and mouth Increased thirst Headache
-
What is Disordered Drinking?
An alcohol problem can affect anyone at any age. Many factors, including job stress, genetics or depression, may contribute to the start of disordered drinking. Drinking alcohol exists on a continuum. For example, if someone feels down in the dumps for some time, it doesn’t mean they are clinically depressed. So if someone goes through a period with above-normal alcohol consumption, it doesn’t necessarily mean they abuse alcohol. Although “alcoholic” and “alcoholism” are common, they are not clinical descriptions. Alcohol use disorder is the preferred term. Symptoms are often mild but can be the start of a more significant problem. According to the National Institutes of Health (NIH), over 16 million adults live with alcohol use disorder. Symptoms of Alcohol Use Disorder Do you recognize any of the following symptoms in yourself or someone you know? Drinking more or longer than intended Trying to cut down or stop drinking but not able to Having to drink more than you once did to get the same feeling Being annoyed when family members discuss your drinking Regretting your behavior while you were drinking
-
Department Spotlight: Imaging
The imaging department is where scientific precision and patient connection come together in harmony to help diagnose a multitude of conditions. When a mystery needs to be unraveled, experts in X-ray, CT, MRI, ultrasound, echocardiography, mammography and nuclear medicine step in to provide a deeper lens into each patient’s inner workings. At Renown Health, our imaging specialists exemplify this and more. With the inpatient teams at Renown Regional Medical Center and Renown South Meadows Medical Center and many outpatient locations across Reno and Sparks, our dedicated and compassionate imaging and radiology technologists make this symphony of healing a melodious reality. Through the lens of their expertise and the state-of-the-art equipment at their fingertips, the invisible becomes visible, pain transforms into answers and the path to recovery. A Picture Tells a Thousand Words Every patient image tells a story, and Renown’s Imaging department is full of master storytellers. From X-rays that capture the intricate architecture of bones to MRIs that unveil the complex structure of organs, these team members use sophisticated techniques to make sure every patient receives the highest standard of care. Within the imaging landscape, no day looks the same – and each team can expect a different set of challenges to overcome, all while helping providers gain better diagnostic clarity. “Every day in imaging is a little bit different, and I love that,” said Savannah Terrana, Outpatient CT Scan Technologist at Renown X-Ray and Imaging – Vista. “We start like everyone else: getting our rooms stocked and ready for patients and protocoling the day's exams. We have a lot of different types of scans, like x-ray, CT and bone density, and a variety of conditions that we are evaluating for the ordering providers, like fractures, cancer, bleeds and more. “When we get into work, we get a daily assignment that decides whether we are in one of our outpatient or inpatient rooms,” added Ireland Bennett, Echo Technologist at Renown Regional. “Then when we are on inpatients, we get our assignments for whether we are assigned to transesophageal echocardiograms, the cath lab or pediatrics. When we are on outpatients, we get a set schedule for the day with patients every hour from 7:15 a.m. until 4:15 p.m. We do our best to be efficient as possible to not delay any patient care or discharges.” “X-rays aren’t just for bones; we do chest X-rays to look for pneumonia and intestinal issues, and we also do fluoroscopy, which is a live video X-rays while patients drink contrast or while surgeons fix fractures with screws and other hardware in the operating room,” said Amethyst Winters, Inpatient Diagnostics Imaging Lead at Renown South Meadows. “There is a lot of variety, and we provide imaging for patients in the entire hospital.” Equipped with advanced technologies and the unique skills they acquired in a trade program, at the university-level or in the military, the Imaging department can deliver precise and comprehensive information to help providers make accurate diagnoses. And their role transcends beyond the image scanner. “A typical day for an MRI Technologist depends greatly on outpatient or inpatient settings,” said Sean Fryer, Supervisor of Imaging for Renown X-Ray and Imaging – Pringle. “There is a lot of screen time and usually in dark areas, but this is where our technologist skill set comes into play – manipulating parameters to either increase quality by signal/resolution or decrease them a little to gain time." “A day in the life as an ultrasound tech would of course be performing ultrasounds on our patient community, but there is much more to it,” added Mary Rushton, Ultrasound Specialist at the Renown Breast Center. “This includes keeping rooms clean and stocked with supplies, protocoling exams and studying patient history so you can give the best patient care possible, continuing education and training to keep up with new technologies and being an aide to your radiologist. Working with many different personalities, you recognize that you cannot complete every step of the patient care process all by yourself – it requires collaboration from your team to give the ultimate patient care experience." Mary brings up an excellent point about the wide variety of people her team meets every day, on both the patient and employee side, with the common goal of solving diagnostic mysteries. This aspect of their work has become one of the highlights of their career. “Working in imaging allows us to meet many members of our community,” Teresa Shutts, Breast Health Coordinator at Renown X-Ray and Imaging – Pringle. “We are responsible for providing imaging exams, managing patient needs and creating a comfortable and caring environment for people who are possibly going through the worst times of their lives.” Along with every day being different, our Imaging team members thrive in their dynamic and fast-paced work environment, where efficiency and urgency are vital, especially among a constant stream of patients in need of timely diagnoses. “Our days in CT are very fast paced,” said Shelly Lavin, Imaging Lead for Inpatient Diagnostics at Renown Regional. “Our modality is the first choice for assessing stroke and trauma patients. We are fortunate to have very competent tech aides who help work up CT orders by checking orders, IV status and labs. We generally have inpatients scheduled every half hour, and we work these around a very full ER list. When we get extremely busy, we have to strategize how we schedule our patients in the various scanners to expedite exams and not delay patient care.” “We provide patient care for those who come in for emergencies, trauma, inpatient care, surgery and fluoroscopy studies,” added Sean Elliott, Inpatient Radiology Technologist at Renown Regional. “I was always told in school that our main purpose was to help doctors better diagnose patients, and imaging provides many modalities to appropriately diagnose.” Behind-the-scenes, our Imaging surgery schedulers are the keys to ensuring each appointment runs smoothly, communicating directly with patients to get their exams off to a good start. “Every day it is my task to make sure we have everything we need to do the exam that is ordered for a patient,” said Isela Gonzalez, Surgery Scheduler for Renown X-Ray and Imaging – Double R. “This includes the order, authorization approval, completing the protocol, confirming the appointment, re-stating the address and directions, going over any prep for the exam and giving them their estimate cost for the exam. I always do my best to give the patient the best experience possible.” Whether they are in the weeds of radiology or in the depths of patient coordination, Renown’s Imaging department is unmatched – and the direct beneficiaries are their patients.
-
Smart Watch Notification Saves a Life
In sailing, when you encounter rough seas, you can’t change the wind pattern, but you can adjust your sails. The same rings true for life. We confront unpredictable circumstances daily, but how we react to them can make all the difference. For Renown patient and avid sailor Robert (Dan) Seifers, recent events make this mantra reign true. A Concerning Alert Monday, Aug. 22, started out just like any other day for Dan. He was on a walk with his dog, enjoying the sunshine, when suddenly he felt a wave of dizziness and a buzz on his wrist. His Apple Watch alerted him that his heart rate had dropped to dangerous levels. Returning home immediately, he notified his wife, Carol. Doing their best not to panic, the couple confirmed the reading with their at-home blood pressure machine. The watch was right – Dan’s heart rate was in the low 30s. After taking some time to see if Dan’s heart rate would return to normal, the couple decided it was time he sought medical help. Conveniently, Carol had a lab appointment scheduled next door to Dan’s primary care physician, Dr. Bonnie Ferrara. The couple headed out the door, not realizing what the rest of the day would bring. The Next 48 Hours Upon arrival at the office, Dan calmly approached the front desk to explain his situation. With no delay, staff members sprang into action, quickly showing Dan to a patient room and notifying Dr. Ferrara. Before he knew it, Dan was receiving an electrocardiogram (EKG). Following a review of the results, Dr. Ferrara returned to let Dan know he needed to get to the hospital immediately. The rest of the afternoon moved quickly for the couple. Dr. Ferrara had already notified the Renown Regional Medical Center Emergency Room staff, who were on standby for the couple’s arrival. “Gee, this must be serious,” thought Dan, who at the time was experiencing no other alarming symptoms other than the low heart rate indicated on his watch. Several doctors and nurses began their analysis, including a chest x-ray, blood test and additional EKG. Confirming Dr. Ferrara’s results, a Renown cardiologists, Dr. Christopher Rowan and Dr. Shining Sun, joined Dan’s care team. Within two hours of checking into the hospital, Dan was admitted, monitored overnight and prepped for surgery to receive a pacemaker the next day. Tracking Your Heart Health Following the purchase of their Apple Watch devices, Dan and Carol were unaware of these heart health features. Like many others, they were looking forward to the next best tech gadget that would help them stay connected with their friends and family. Now, the couple says they will use their experience to spread the word about the importance of ensuring these settings are enabled. According to Apple, you can turn on these notifications from the Heart Rate app on your Apple Watch (Series 1 or later) to alert you to high or low heart rates and irregular heart rhythms. If you receive a notification, an irregular rhythm suggestive of atrial fibrillation (A-Fib) or a low or high heart rate has been identified and confirmed with multiple readings. In Dan’s case, the signal from his watch was the result of a heart block, a condition where the electrical signal that controls your heartbeat is partially or completely blocked. Dizziness and low heart rate are common symptoms of a heart block. But this was not the first time the couple had experienced this type of alert from their watch. More than a year and half ago, Carol’s watch notified her of an irregular heart rhythm that was suggestive of A-Fib. She immediately made an appointment with Dr. Danish Atwal, the lead cardiologist at Renown’s Helaine Greenberg Women's Heart Center. Thanks to medication prescribed by Dr. Atwal, Carol now lives a healthy, active life while managing her A-Fib, continuing to wear her Apple Watch, which can also help track her A-Fib History. “I’ll share our story with anyone who will listen and encourage them to get a smart watch. I consider myself an unofficial spokesperson,” said Carol with a chuckle. A Thankful Heart The Senior Care Plus members could not be more amazed at the way Dan was treated by the staff at Renown. “I wish I could personally thank them all. I will highly recommend Renown to all I come in contact with,” said Dan with his Apple Watch still proudly strapped to his wrist. “I was closely monitored and treated like royalty.” Quick action to medical emergencies like Dan’s is just one of the many reasons why collaboration is part of our four key values at Renown. The open line of communication between our primary care facilities and hospitals helped Dan get the prompt care he needed, right when he needed it. A month post-op, Dan is doing well and back to enjoying the things he loves during his retirement, including playing the harmonica in the Grumpy Old Man Band, exploring the northern Nevada backroads in his jeep and working on his swing at the golf course. Dan can rest assured that while enjoying the winds of life, if his heart begins to beat too slowly again, the pacemaker will send a signal to correct the beat. “The prompt attention to my heart block undoubtedly saved my life,” said Dan in what he calls his 6-star review of Renown Health. “Thank you from the bottom of my heart, which is happily beating at 60 beats per minute.” This article is not sponsored by or affiliated with Apple, Inc. For more information on the Apple Watch and it's features, visit apple.com.
-
Department Spotlight: Emergency
The emergency department is a central part of Renown Health’s hospitals. Serving patients in need of emergent attention, this team has an incredible level of dedication to not only tending to emergencies big and small, but also saving lives 24 hours a day and seven days a week. This critical work happens daily at Renown Regional, Renown South Meadows and Renown Children’s Hospital. Patients in Renown’s emergency rooms (ER) are in the best hands, and it is all thanks to the devoted, hard-working teams who run the show. Saving Lives Around the Clock As the only Level 2 trauma center between Sacramento and Salt Lake City, taking care of a constant stream of patients in the Renown Regional, Renown South Meadows and Renown Children’s ERs come naturally for these teams. Whether it be 3 a.m. or the lunch hour, this team is always ready to spring into action to attend to virtually any health emergency under the sun. According to Gabby, an RN in the Renown Regional ER, everyone in the ER must be ready for anything. “We are the first line of care that the patient receives before they are admitted or discharged,” which means the team sees a wide variety of emergency situations each day. Patients rely on the ER to protect them and help them heal from severe conditions. From head injuries and broken bones to heart attacks and strokes, this team has seen it all at every time of the day and night. “The ER is an uncontrolled, unpredictable environment,” said Miriam, an RN in the Renown Regional ER. “It’s essential that we all are ready to jump in and help at any time.” Beyond the general ER at Renown Regional, Renown Children’s Hospital is the only accredited Children’s Hospital Emergency Room in all northern Nevada. The first and only facility of its kind in the Reno-Tahoe region, this robust emergency department is equipped with pediatric specialists and child-sized equipment to give children the highest level of support. “We are proud to keep a fun atmosphere with vibrant colors to help our young patients ease their anxieties, making them as comfortable as possible while providing excellent care,” said Ginger, Manager of Nursing for Renown Children’s ER. While the majority of patients are treated onsite and discharged that same day, several ER patients get admitted to the hospital, when that happens, the emergency department works quickly with the Renown Transfer and Operations Center (RTOC) to get patients in a bed as soon as possible. All day and all night, ambulances and helicopters deliver members of our community in need of care. But never fear – our incredibly capable emergency department is here. Kicking off into immediate action is a core requirement for the emergency department, and it is a task the entire team has nailed down to a science. Team Tenacious When asked about their team, members of the emergency department echoed the same notion: “I am not alone.” The emergency department never leaves their colleagues out to dry, and in an emergency environment, always being able to lend a hand whenever needed is vital. For Ashley, an RN at Renown Regional, one of the main reasons why she continues to work at Renown is because of her colleagues, along with a myriad of resources and state-of-the-art technology that are at their disposal. She adds, “It is such a joy to come in to work alongside my team.” Amy, Supervisor of Nursing for the Renown South Meadows ER, feels the exact same way. “Being an emergency department, we sometimes see things you don’t always see every day,” said Amy. “It’s a relief for our patients to know that they are in the best place in the region for their care. I credit all of that to my team.” As our emergency room capabilities continue to grow, this also includes our Children’s Hospital ER. Last year, the William N. Pennington Foundation provided a $7.5 million gift to the Renown Health Foundation to keep pediatric care – including pediatric emergency care – closer to home and expand our availability to our youngest patients. As reported last year, Dr. Joseph Gassen, a pediatric emergency doctor with Children’s Hospital, was the only pediatric emergency physician in the region as of 2021. Thanks to this gift, he was able to move to Reno to provide care in the Children’s Hospital ER. “The hospital is dedicated to improving the care of children in northern Nevada, and I wanted to be a part of this amazing vision," said Dr. Gassen. “I would not have been able to relocate to Reno without the support from the hospital and the William N. Pennington gift.” Besides achieving optimal outcomes for their patients, their efforts also paid off in the form of awards and recognition. Internally, the emergency department recognizes Employees of the Month for their outstanding work. Recently, Renown Regional Emergency Physician Dr. Patrick Russell and Claire, an RN, were recognized with this honor. Outside organizations have also noticed these exceptional team members. The Reno Gazette Journal’s recognized the Renown Regional ER as the Best Emergency Room in the 2022 Best of Reno Awards, complimenting Renown Regional’s wins as the Best Hospital and Best Place to Have a Baby. The tenacity of the emergency department continues to surpass expectations, and their published achievements only scratch the surface of what is sure to come. A Growing Team of Heroes To continue meeting the growing need for emergency care regionally, especially when it comes to trauma and children’s services, the emergency department is looking forward to welcoming new team members. For those looking for a fast-paced, team-oriented atmosphere and the opportunity to be on the healthcare frontlines, the emergency department is a perfect fit. As teamwork is clearly essential, the emergency department is an ideal environment for someone who is “not afraid to ask questions and always eager to learn new things,” according to Miriam. While one staff member’s patients may be settled, staff one assignment over could be overwhelmed with patient volume, so it is an imperative skill for a colleague to be a self-starter and take the initiative to help wherever needed. Bryan, an emergency trauma technician at Renown Regional, emphasizes this point, adding, “A good colleague is one that knows you well and can infer your body language. They know how to read a situation and pre-plan for the next step. Being attentive, a valuable resource and knowledgeable about patient populations – that's the works!” Career growth and lifelong learning are important to this group, so career-minded individuals will be in good company in the emergency department. “I choose Renown so I can jumpstart my career as a nurse in the top ER in the region,” said Gabby. This team is always learning and always on top of the latest research – which only further solidifies Renown’s place as the preeminent ER in northern Nevada and northeastern California. If you take one thing from this article, let it be these parting words from Amy: “These are some of the smartest, most devoted individuals you will ever meet, and we are so lucky to have them serving our emergency department. You will only regret not working with this team.”
-
The Pieces of the Puzzle: Thonet LaBadie’s Breast Cancer Journey
“A breast cancer diagnosis begins much like a jigsaw puzzle to be worked through. It’s an overwhelming mess of scattered pieces that make no clear sense, poured out of the box into a crumbling pile of confusion. But slowly with persistence, focus, determination, a positive attitude and working through the challenges day by day and piece by piece, they in time both become whole and beautiful again.” – Thonet LaBadie On Feb. 13, 2015, Thonet’s life as she knew it took a drastic turn. In just one moment, everything shifted. The happy and healthy wife, mother of 17-year-old twins, former teacher and immunization specialist was about to face the fight for her life. That fateful day nearly a decade ago was when she received the unsettling news: she had breast cancer, and it had metastasized to her lymph nodes. Though she was faced with a daunting diagnosis, Thonet’s positive spirit and zest for life never wavered. Never did she think, “why me?” Nor did she think, “I’m not strong enough.” Her thought process was quite the opposite – “I am going to ride this rollercoaster until it stops, and I walk away cancer free.” With her loving family and friends rallying behind her, as well as her expert Cancer Care teams at Renown Health and Cancer Care Specialists (formerly known as Reno Oncology Consultants), Thonet knew that her journey would not be traveled alone, and she was determined to defeat cancer once and for all. She promised her daughter Jourdyn she would stay strong and not give up the fight. The Unexpected Discovery Thonet did everything she believed was right in her preventative healthcare journey. She lived an active lifestyle, she filled her life with love and happiness, she did not have any genetic markers for breast cancer and never missed a preventive check-up. Someone like her shouldn’t develop such a debilitating disease, right? As it turns out, she was told by professionals that with this disease, it’s become more often not about who develops breast cancer – but when. Breast cancer makes up for about 30% of cancer diagnoses in women across the U.S. So, when Thonet felt a lump in her breast in Nov. 2014, she knew she had better play it safe than sorry. She took her concerns to her doctors, who ran all the necessary tests. The unfortunate result: invasive ductal carcinoma (stage 2B), the most common form of breast cancer. Though Thonet was terrified, she was also tenacious. She was ready to Fight the Good Fight right then and there. Thonet chose to undergo a bilateral mastectomy. So that’s precisely what she did in April 2015 at Renown Regional Medical Center. Thonet was ready to put breast cancer behind her, but unfortunately, the trek was just beginning. During her mastectomy, her care team tested her lymph nodes. Four were removed. What came next was her most valiant fight of all: chemotherapy coupled with radiation, as well as more reconstructive breast surgeries along the way. Courageous Connections With 36 radiation treatments, 8 rounds of chemotherapy, 6 surgeries and 1 brave spirit, Thonet's healthcare journey has been nothing short of vigorous. Fortunately, she had an expert oncology team on her side every step of the way. And it goes even further – Thonet’s college acquaintance Dr. Jennifer Sutton, an oncology physician at the William N. Pennington Cancer Institute (formerly the Renown Institute for Cancer), was her radiation oncologist. She felt comfort knowing that a significant aspect of her care was in the hands of a trusted physician and a team of loving nurses, cancer care navigators and radiation therapists, whom she calls the “Renown Radiation Rockstars.” Thonet felt an immense connection not only to her warm and welcoming care team but also the other oncology patients she met along the journey. Patients facing cancer often receive radiation treatments several times a week, so Thonet had a chance to make close relationships with the other patients who were on a similar path as she was. Throughout her treatment process, Thonet participated in cancer support groups, which she believes are vital for anyone diagnosed with the disease. “Had it not been for my diagnosis, I would have never met all the amazing people I did at Renown and beyond,” she recalls. “At the end of my treatments, I knew I was going to miss them.” The love and support of Thonet’s care team, fellow patients, family, friends and community helped her remain positive throughout the entire process, always focusing on the positive – even during the most physically and emotionally tolling parts of treatment. Crossing the Finish Line Every day brought a new obstacle to overcome, whether it was a treatment, a side effect or an emotional response to the intense journey. Thonet’s motto throughout it all was “day by day, one foot in front of the other, from start to finish.” In Dec. 2016, Thonet finally made it to that finish line. With the completion of chemotherapy and radiation behind her, she walked out the front doors of the Pennington Cancer Institute, threw her fist in the air in excitement and finally got to revel in the fact that she had her health back. She had survived. Inspired by her journey and her breast cancer “sisters” she met while in treatment, Thonet wanted to give the same level of care and attention she received back to her fellow community members battling cancer. She proudly serves as a breast cancer “angel,” offering comfort and support to those who need it most. Thonet is also looking forward to the completion of the Pennington Cancer Institute’s Conrad Breast Center, currently under construction at Renown South Meadows Medical Center, noting how important it is for breast cancer patients to have expanded access to crucial cancer care in south Reno. Today, at nine years cancer-free, Thonet is thoroughly enjoying her life. She loves traveling, spending time with family and seeing her now-adult son and daughter thrive in their own lives. She also recently underwent hip replacement surgery and is proud to be back on her tandem bike with her loving husband of 33 years, Mike, who she credits for his never-ending support in sickness and in health. “No looking back – only forward to healthy living. Onward!” Thonet exclaims. And for anyone out there going through cancer treatments, Thonet has some words of wisdom to take to heart: “Cancer chose the wrong person when it tried to tackle us. Stay strong and fight on, day by day. On even the most difficult, darkest day, remember that you are stronger than you know.”
Read More About The Pieces of the Puzzle: Thonet LaBadie’s Breast Cancer Journey
-
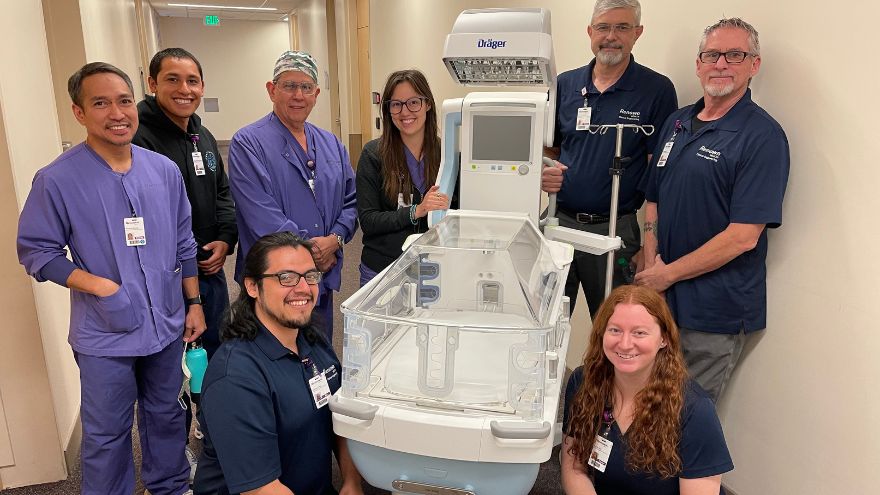
Department Spotlight: Clinical Engineering
Renown Health strongly supports and advocates for innovative medical technology. Our diverse lineup of medical equipment enables our care leaders to provide quality care to every patient. But what if a piece of technology breaks down? What happens when our care teams are ready for technological upgrades? Where do employees go when they have a question about a complicated piece of equipment? Enter the Clinical Engineering department. This sophisticated team is staffed with intelligent, science-minded individuals who are ready to jump in and help at any given second. From newborn incubators to robots that clean the hospital floors, these team members are the med-tech masters that keep our health system running. Equipment Experts Upon entering the Clinical Engineering department’s workshop, you are welcomed with an abundance of high-tech equipment undergoing repairs and upgrades. The department takes care of more than 26,000 pieces of equipment throughout the entire healthcare network, including the technologies at the University of Nevada, Reno School of Medicine, which they just took over this past year. To the average person, this may seem overwhelming; however, for this team, this is the exact environment they thrive in to make the technology magic happen. “I am motivated and engaged every day at work,” said Tony Martinez, Supervisor of Clinical Engineering for Renown. “Our department is fast-paced and rewarding, and that’s a big plus.” While some team members enter the department as equipment generalists, this team offers training to develop their skills on certain pieces of equipment, eventually becoming specialists. “Every month, we encourage our colleagues to undergo specific training on more delicate equipment,” said Tony. “Once we get to that point in their training, we assign different equipment to our team members every month. They pick up the experience very quickly.” As a Clinical Engineering Technician for Renown, Rylie Nickerson took advantage of the training and educational opportunities offered to her and is now a ventilator specialist especially for Renown’s neonatal intensive care unit (NICU). “Regardless of whether I’m working on ventilators or on another piece of equipment I’m assigned to, I’m always thinking about how I can help the patients, nurses and doctors,” said Rylie. Raul Hernandez, a Clinical Engineering Specialist for Renown, is the go-to person for anesthesia, heart-lung bypass, red cell saver and life support equipment. He embraces the fact that, regardless of whether you are a specialist or a generalist, there is no typical day working in this department. “Every day brings different challenges,” said Raul. “I really enjoy the mental exercises I do every day. They keep me grounded and focused.” On top of their day-to-day work and any special projects or emergencies that come up, the team is on an ongoing preventative maintenance schedule. Think of this work like your car’s oil change – routine maintenance to prevent something from breaking down in the future. “At any point, we might have 100-200 extra pieces of equipment to handle during preventative maintenance,” said Taylor Gray, a Clinical Engineering Technician for Renown. “We are always helping each other through any issues.” Our Clinical Engineering team shows exactly what it means to be collaborative. Even though their to-do lists are ever-growing, this team never feels alone. They know they can always lean on each other for support, regardless of the workload. “We always have each other’s backs,” said Taylor. “I feel so happy and satisfied in my job, and my coworkers are a large part of that.” Celebrating the Genuine Difference The Clinical Engineering department is driven by their desire to help and take care of the entire health system, and in turn, make a genuine difference for the communities we serve, from the medical staff to the patients. “The satisfaction you get in our field when we impact patients’ lives and their healing process is so motivating and engaging,” said Tony Martinez. “It’s a great feeling.” The team knows the common saying ‘Walk a mile in someone’s shoes’ very well; so well, in fact, that they take it to the next level, doing everything they can to prevent frustrations and extended down times. “We try to walk a mile in someone’s shoes before they get angry,” said Reagan Jordan, Director of Clinical Engineering for Renown. “Your satisfaction is our mission, and our team continually works to improve their outcomes every day.” This department is where the entrepreneurial spirit and science-focused mind meet. For people like Raul Hernandez, who came from a business background as well as decades of medical technology experience, Renown helps him bring both his personal and business skills into focus. “This environment is very beneficial for Renown, me, and of course, the patients,” added Raul. Being members of a team that is committed to excellence and purpose inspires them to reach new heights in patient care. “I am constantly reminded of the positive impact we have by witnessing the individual experiences we have and hearing the enthusiasm and thankfulness in their voices,” said Raul. “It gives me a great sense of pride to work at Renown.” "There is a strong feeling of mutual respect here,” added Ed Trejo, a Clinical Engineering Technician at Renown. “We are always here to help.” The proof is in the data. The Clinical Engineering team scored as one of the top departments in the recent Renown employee engagement survey, with their results sitting at more than 94 percent. “This speaks to not only our department leadership but also the team as a whole,” said Reagan. “I am extremely proud of them. Despite the pandemic, they are knocking it out of the park.” For this department, coming to Renown is easy; staying at Renown is even easier. “Staying at Renown is the easy choice,” said Raul. “And this team is only going to grow.” Workflow Whizzes and Kindness Champions “Rolling with the punches,” as Tony Martinez says, comes naturally to the Clinical Engineering team. With the constant workflow of equipment coming into the shop, every team member has learned how to be experts at prioritizing, especially based on the needs of our organization. Even though their jobs can bring a lot of intensity, this department’s positive attitude radiates throughout the hospital. Upon entering the workshop, everyone is greeted with a smile from every team member, along with an immediate willingness to dive into the complex world of engineering. “The experience of helping other people with their unique needs is invaluable,” said Taylor Gray. If this work environment sounds enticing, great news – the Clinical Engineering team is growing. Motivated, aspiring engineers with a passion for healthcare and an associate’s degree in a related field are welcome. Military experience is also valued very highly in this team. As many of our military servicemen and servicewomen gain specialized engineering experience while enlisted, the military-to-engineer career ladder at Renown is especially strong. In fact, according to Paul Joseph, a Clinical Engineering Technician at Renown, the majority of their teammates come from a military background. Above all, being capable of prioritizing on the fly, thinking critically, having an open-mined outlook and being self-driven are the top skills that this department values. As Ed Trejo states, “If you’re willing to wear different hats, you will do very well here." “Go with the flow, and expect the unexpected,” added Rylie Nickerson. Those who join this team feel at home. The warm embrace of the team’s kind nature and the supportive environment they all foster inspires an efficient workflow that helps our entire hospital system function at the top of its game. At the end of the day, everyone who joins the team, or anyone who even interacts with the team in any capacity, will be in good hands. Mandy Noriega, a Clinical Engineering Technician for Renown, closes these thoughts with a great reminder to each and every one of us: “After all, teamwork makes the dream work.”
-
Department Spotlight: Vascular Access at Renown Regional Medical Center
Our bodies hold a special elixir to life that keeps our brains thinking, our lungs thriving and our hearts ticking – blood. The bloodstream is key to making sure nutrients, hormones and oxygen all get to the right place and transport waste out of the body. However, blood can be sensitive. Entering the bloodstream to help your veins, arteries and vessels function or give medication directly to your vascular system is a delicate process. It takes the careful hands and minds of compassionate healthcare professionals to make it all happen. At Renown Regional Medical Center, those professionals make up the Vascular Access department. Proud members of the region’s leading vascular care team, our Vascular Access nurses are each hospitalized patient’s bedside bloodstream companions. Access for Life The nurses in our Vascular Access team do exactly what you’d expect: provide access to the bloodstream for medications and other medical interventions. These team members are specialists in assessing, placing and managing devices for patients needing IV treatments, blood draws, hemodialysis and more. The devices they work with, otherwise referred to as vascular access devices (VADs), run the gamut of vascular excellence. These include: Peripheral inserted central catheters, also known as “PICC lines” Hemodialysis catheters Peripheral IV catheters (PIVs) Central venous catheters (CVCs) Long-term peripheral catheters, also known as “midlines” In Vascular Access, time is of the essence. Their daily life at work involves working quickly and accurately to ensure patients get the best possible outcomes. “Our day starts off with prioritizing orders,” said Kimberly Wallace, Vascular Access RN. “It is important to us that patients get meaningful care in a timely manner so that they can proceed with discharges, receive important medications and proceed to exams. We juggle timelines to get patients’ access as quickly as possible.” “You’ll find us rolling around the hospital with our ultrasound machines and placing PICC lines, midlines and PIVs, as well as helping out with dressing changes and line audits,” added Derek Zastre, Vascular Access RN. When it comes to complex vascular procedures, providers around Renown feel confident that they can call upon our talented Vascular Access team to handle it with the utmost care. “We receive orders from providers for central lines, midlines and difficult IVs,” said Kris Gregor, Vascular Access RN. “We prioritize and assess need by evaluating patients' charts and ensuring the correct line is ordered and subsequently placed.” Even more PICC line experts can be found at Renown South Meadows Medical Center, where the Vascular Access department has five Imaging PICC Line nurses, nuclear medicine nurses and MRI nurses ready to serve with their careful hands as they precisely place these flexible catheters to administer life-saving medications. Stay tuned for their Department Spotlight in 2025! Naturally, a procedure that involves entering the bloodstream can be quite intimidating for any patient. Luckily for them, empathy comes easily for the Vascular Access care team. “We walk our patients through the process, explaining the reasons why we are placing the lines and how it is going to feel,” said Kris Gregor. “We try our best to alleviate fears and anxiety by maintaining professionalism and showing empathy. Generally, patients relax while we place [the lines] and report that it was not as scary or as bad as they had thought it would be.” “We explain the procedure to the patients, discuss pain control that will be given during the procedure and help the patient find a comfortable position,” added Kimberly Wallace. “We ask them about themselves and get to know them. Some patients want to listen to music while the line is being placed, so we facilitate these types of comforts for them. We provide them with opportunities to ask questions.” Each patient’s hopes and wishes about their care are always top of mind for the Vascular Access team, every step of the way. “We place a lot of PICCs and midlines to better our patients' outcomes all over the hospital,” said Kris Gregor. “We always have our patients' best interest at heart.” Up for the Challenge Being a Vascular Access nurse is not for the faint of heart. A steady hand, a careful approach and precise attention to detail are all musts. The Vascular Access team is not only up for the challenge, but they are also masters of the challenge. It’s a badge of honor for them. “I am honored to be a part of a crew that takes infection prevention seriously, has no reported central line associated bloodstream infections (CLABSIs) from the line placement and takes peer education seriously,” said Derek Zastre. “We inform everyone of the vascular access policy for line placement.” “I am also very proud of our team and the work we are doing to reduce CLABSIs in the hospital,” added Kimberly Wallace. One of the many benefits of this team is their diverse array of experience prior to becoming Vascular Access RNs, from the ER and ICUs to the lab. “I am an ER trauma nurse who has worked in the Cath lab, post-anesthesia care unit (PACU) and flight nursing. Vascular Access seemed like a great way to specialize in accessing difficult veins and placing lines,” said Kris Gregor. “I have an extensive history as a phlebotomist before becoming a nurse, and Vascular Access just sounded right up my alley,” added Derek Zastre. “I have loved every minute since joining the team.” A common theme among this team is the appreciation they have for the opportunity to help both patients and their fellow nurses and providers. They are true advocates for both their patients and coworkers. “I have worked at Renown for 15 years. I started in the general surgical unit (GSU) and became an ultrasound trained RN after three years,” said Kimberly Wallace. “Vascular access is very important to both patients and care providers. I have always found myself drawn to vascular access and not only helping other nurses on my unit gain meaningful access but also [nurses] on other units. It can be a big source of anxiety for both. I joined this team in 2020 and have loved it ever since.” No matter the case, our Vascular Access professionals will never falter in their passion for their work. Regardless of how challenging the procedure may be, they are proud to rise to the occasion. The Renown Promise Working for a hospital or health system can be one of the most fulfilling career paths someone can take, especially for those who are passionate about helping people. Working for Renown, however, takes fulfilling careers to a whole new level. But don’t just take our word for it – take it from our Vascular Access department. “I have worked at Renown my entire nursing career, and I continue to work here because I love my coworkers and the opportunity to make a genuine difference every day I come to work,” said Kimberly Wallace. Many of these team members were inspired to continue serving at Renown after completing a nurse apprenticeship or new graduate nurse position, especially after receiving such strong support from their coworkers and leaders, both personally and professionally. Landing in Vascular Access was the cherry on top of an overall great experience working for Renown. “I really enjoyed my nurse apprenticeship in the ICU and my first year working in ICU. I enjoy the culture of learning and the teamwork here at Renown,” said Derek Zastre. “When I had issues in my personal life and needed to change directions in my nursing career, my supervisors, educators and directors were awesome and so gracious in helping me find something that fit my needs. I ultimately landed in Vascular Access with an awesome crew and leadership that provides flexibility and support.” “I was a new grad here in the ER and have moved away from the region several times, but I always come back,” said Kris Gregor. “I really like the camaraderie and how the doctors are so amiable to work with.” With strong sense of unity, unique patient care opportunities and engaging challenges that inspire, it’s not a matter of “why” the Vascular Access team wants to work in their department – it's more so a matter of “why not?” “Vascular Access is the BEST,” closes Derek Zastre.
Read More About Department Spotlight: Vascular Access at Renown Regional Medical Center
-
Department Spotlight: Hospice & Palliative Care
In the book of life, everyone eventually reaches the final chapter. End-of-life isn’t often something a patient or loved one wants to think about. The end of someone’s life isn’t a final option – it's a privilege. At Renown Health, we have a compassionate team prepared to approach this privilege with kindness and care. The Hospice & Palliative Care department at Renown is the best of the best. Their efforts go far beyond simply addressing physical pain; they also bring emotional and spiritual solace to patients and family members navigating the complexities of serious illness and end-of-life. This team provides crucial guidance and expert knowledge, comfort and care when it is most needed. Bringing Dignity to the Final Days Contrary to popular belief, hospice and palliative care is not a “last resort” option for families. In fact, it’s quite the opposite. These caring professionals work hard to ensure a patient’s final days are free of pain and full of peace, rather than focused on the end. This type of care isn’t a death sentence – it's a living gift. Each patient is involved in his or her own end-of-life process. They have a huge role in deciding on their own and with their family members how they want to live out their remaining days. “Every team member’s daily work focuses on how to facilitate a good death for each patient,” said Tanya Prosch, Hospice Supervisor. “Ultimately, it is up to each patient’s family to be involved in this process. Every day, there is a lot of communication among team members as we prioritize the needs of our patients. As patients decline and their symptoms change, we continuously assess what topics we will discuss. This creates a beautiful back-and-forth dynamic among the team, patients and families.” “Together, we come as a team to provide what they need, ensuring individualized care for each patient and family based on their safety and specific needs,” added Rachel Schneider, Transitional Care Specialist. “Our care plans are not cookie-cutter; they are tailored to fit each unique situation.” The hospice team provides comfort and support to those in the final stages of a terminal illness. Hospice is focused on one main goal, which is enhancing quality of life for patients and their families. “In general, hospice staff conduct home visits to see our hospice patients,” said Amy Nieminen, Manager of Home Health & Hospice. “We have an interdisciplinary team that includes nurses, aides, chaplains, social workers and volunteers. Together, we address both the physical and emotional, spiritual and social needs of our patients and their families at the end of life, ensuring they have a meaningful and peaceful experience. We do a lot of work with families and loved ones, providing follow-up calls and support for the patient’s caregivers after their passing. Our support extends for up to a year, with grief specialists available to help families through their loss. Additionally, we have rotating on-call nurses every night and weekend, so patients are never left without care.” While palliative care shares similar duties to hospice care, it differs slightly. Palliative care can be involved at any stage of a serious illness, even during treatments. “During in-home palliative care, we work with patients who may be physically ready for hospice but who are not yet psychologically, emotionally or spiritually prepared to make that transition,” said April Lennon, APRN for In-Home Palliative Care. “They may still be exploring treatment options and working with their specialists. We provide a lot of support, helping them understand the consequences and benefits of various treatments. Additionally, we focus on symptom management for patients experiencing significant pain or nausea, assisting them in managing these symptoms effectively.” On both sides of this department, the team has the opportunity to be especially involved in their patients’ lives and in the lives of their families. Giving loved ones more time with their relative facing end-of-life is a duty that these team members take seriously. “My job is to educate families about what’s coming next and what is happening now, as there is a lot that occurs during the death process,” said Katie Adams, Hospice Nurse Case Manager. “Families will never regret the time and effort spent during this process. We have only one chance to get this right. This is not just a random hospitalization that people will forget; it is a significant moment that everyone around the patient will remember.” “Being able to connect more deeply with patients’ and families’ stories and their narratives about life is essential, as it provides a broader understanding beyond just the medical picture of what is happening,” added Libby Krayk, APRN for Hospice. “We explore their expanded value and belief systems to assist with decision-making, helping them make choices together. When patients are no longer distracted by pain or nausea, they can focus on their long-term desires and goals and spend more time with their families." “Crisis intervention, social work, education, family conferences, and placement issues are all part of what we do, and it’s quite exciting,” added Donald Kamka, Social Work Care Coordinator. “You become fully invested in the lives of those you help, which is what makes this job so rewarding. This is a remarkable time in their journey, and it’s evident that everyone involved has a vested interest in it." Naturally, many questions, worries and fears arise during this time in a patient’s life. The Hospice & Palliative Care team members are expert communicators and know exactly how to relieve some of those anxieties, prompting a more peaceful end-of-life. According to this team, it’s all about transparency and compassion. “Our role involves helping patients navigate the healthcare system as they face death,” said April Lennon. “Home visits can range from one hour to three hours, depending on the needs of the patient and their family. We engage with entire families, including those who are out of town, coordinating care and working with many providers in the area. Our hope and goal for every patient is to ensure they understand what they are doing and why they are doing it, empowering them to make their own choices.” “We often find ourselves addressing the most difficult information, which can sometimes be seen as the ‘elephant in the room’ that people tend to avoid,” added Libby Krayk. “I ask patients for their permission regarding what they want to know and who they would like involved in the conversation. This approach can help alleviate some of the challenges and stress they may be experiencing. Being honest and discussing matters in a way that they can understand is essential. I take the time to sit down with my patients and connect with them on a human level, rather than just a medical level.” As a not-for-profit health system, volunteers are at the core of our mission delivery. They graciously dedicate hours out of their week to be a friendly source of help for patients. Renown’s Hospice Volunteers exude this level of kindness and more. Our employed team members attribute their volunteers as a major source of success for Renown’s hospice program. “I believe that being a volunteer provides a role that patients perceive as non-threatening,” said Linda Derry, Hospice Volunteer. “As volunteers, patients feel more comfortable talking to us and sharing things. This dynamic allows them the freedom to express not only how they are feeling but also their fears and any other concerns they may have. It is in these moments that we can truly connect with them, as we are volunteering out of a genuine desire to sit and visit with the patients. “When I see a patient, the focus depends on their specific needs,” added Luanne Geissler, Hospice Volunteer. “I often give family members some time to themselves to do whatever they need to do while I visit with the patient. Many of them are very talkative and eager to share their stories. For instance, one patient told me how to make a baked potato while out in the wilderness, which has become one of my favorite stories. Another patient shared her experiences about coming to America from Asia, discussing her church, her religion and her passion for baking. She would even bring bread to her doctor.” “I have one patient whose main desire is to play chess; he has been playing for over 80 years and is still able to play very well,” added Hervey Ibarra, Hospice Volunteer. “When I visit another patient at his home, we engage in conversations about a variety of topics. Additionally, some patients ask me questions about the military and law enforcement. Whatever they want to do and discuss, that is what I focus on during our time together.” Regardless of whether they are a provider, supporting team member or a volunteer, every person on the Hospice & Palliative Care team shares a primary focus: helping patients live their remaining days, no matter how long that may be, with dignity and comfort, surrounded by their loved ones.
Read More About Department Spotlight: Hospice & Palliative Care






.png?rev=68adc4a5202c439194bbb9e6824080ed)
