Search
Results for 'doctor'
Clear-
Governor Sisolak Signs Senate Bill 342
CARSON CITY, NV – Today, Nevada Governor Steve Sisolak signed Senate Bill 342 into law. The bill authorizes the Nevada System of Higher Education (NSHE) Board of Regents to enter into an agreement to affiliate with a publicly or privately- owned medical facility or related entity, whether for profit or not for profit, to further promote and enhance a medical education or health education program at a university. "Throughout the pandemic, we have relied on doctors, nurses and medical professionals to care for Nevadans in need. Legislation like this will help strengthen existing partnerships in the State so we can recruit, train and keep more medical professionals in Nevada,” said Gov. Sisolak. “I look forward to these continued partnerships to help our state for years to come.” Governor Sisolak was joined by University of Nevada Reno President and former Governor Brian Sandoval for the bill signing. “I wish to thank the members of the Nevada State Legislature and Governor Steve Sisolak for their support of this bill,” University of Nevada, Reno President Brian Sandoval said. “This collaborative and forward-thinking framework will provide cutting-edge patient care delivery, greater clinical research opportunities and will ensure that the next generation of medical providers in Nevada will receive the highest possible training. As the past year-plus has demonstrated, the health care environment in our state and throughout the country continues to be dynamic. The passage of this bill ensures that Nevada has the proactive tools to look to the future, so that we can meet our health care and medical education challenges.” “I appreciate and am so pleased that Governor Sisolak and the legislature approved Senate Bill 342 today, which provides support for integrating the University of Nevada, Reno School of Medicine with Renown Health,” said Anthony D. Slonim, MD, DrPH, FACHE, President and CEO, Renown Health, who was present at today’s signing. “This partnership will improve the health and healthcare of Nevadans and all of the communities that we serve. With this new level of affiliation, we will be able to drive innovation, research, medical education, grant funding for public health, clinical trials and integrate our medical practices to improve access and affordability of care. Together, we are excited to create a healthier Nevada.” “We are so appreciative of the unanimous support of the legislature and now the Governor’s signature and support of this bill that provides guidance to the NSHE Board of Regents as it considers the approval of this critical affiliation between UNR Med and Renown Health. We are excited to move to the next step of seeking approval from the Board of Regents for the affiliation and the establishment of an integrated health care system that will enhance medical care delivery and medical education, will improve health care, and will benefit the health and well-being of all Nevadans,” said University of Nevada, Reno School of Medicine Dean and Vice President, Health Sciences, Thomas L. Schwenk, M.D. “The opportunities to take medical care, medical education and clinical research in Nevada to an entirely new level are unlimited and we thank Governor Sisolak for moving us to the next step in this endeavor.” Photos from the bill signing can be requested from the Nevada Governor's Office. In addition, Governor Sisolak also signed the following bills today: Senate Bill 17 - Revises provisions governing the renewal of certain instruction permits to operate a motor vehicle or motorcycle. Senate Bill 23 - Revises the boundaries of the area from which certain members of the State Conservation Commission are appointed. Senate Bill 53 - Authorizes the Administrator of the Division of State Parks of the State Department of Conservation and Natural Resources to organize the areas under the jurisdiction of the Division into regions. Senate Bill 65 – Revises provisions relating to the composition and administration of the State Department of Agriculture. Nevada Governor's Office Public Relations Media Contact E: press@gov.nv.gov
-
The Greatest Gift of All? A Fully Vaccinated Family!
Renown joins Washoe County Health District to Offer COVID-19 Vaccines to Children 5-11 at Vaccine Clinics. Renown Health is partnering with the Washoe County Health District to help distribute the initially available, limited supplies of an age-appropriate dose of the COVID-19 Pfizer-BioNTech vaccines to children ages 5-11. At this time, all residents 5 years and older are eligible to receive a vaccine. Renown announced today that for parents/guardians with proxy access for their children through the Renown MyChart app, vaccination appointments are now available for children ages 5-11. Pending supply, Renown expects to be able to vaccinate 1,600 children with the 2-dose series in a limited series of weekend clinics. At this time, due to limited supplies, no vaccines for children are available through Renown Medical Group pediatric offices. Vaccine appointments may only be scheduled through the Renown MyChart app; please do not contact a Renown doctor/health care provider or the Engagement Center at this time. There is no cost to establish a Renown MyChart account, and you do not need to have a Renown provider to enroll. For MyChart Technical Support, call 775-982-2781. Renown is covering all costs of the vaccine, and it is offered free of charge. “As a pediatrician, an intensive care physician, a public health practitioner and a grandparent, I encourage parents to vaccinate their children against COVID-19 now. No child should suffer, be hospitalized or die from a disease that can prevented by simply getting a shot,” says Tony Slonim, MD, DrPH, President & CEO of Renown Health. “We remain steadfast in fighting the good fight for our community, and that includes protecting kids. Being able to serve kids and their parents, with the only Children’s Hospital in northern Nevada, and being able to administer COVID-19 vaccines to children is incredibly gratifying for our team. This vaccine will prevent deaths, ICU admissions and will prevent significant long-term adverse outcomes in children." “I tell parents, get your kids vaccinated now- because every kid is at risk,” says Kristina Deeter, M.D., MBA, Pediatric Intensivist, and Vice Chair of Pediatrics at Renown Children’s Hospital. “Please get your family- including your kids, vaccinated now to keep your family safe. Being fully vaccinated and being able to hug Grandma and Grandpa at the holidays may be the greatest gift of all this holiday season.” “The CDC recommends everyone ages 5 and older get a COVID-19 vaccine to help protect against COVID-19. Widespread vaccination for COVID-19 is a critical tool to protect everyone, especially those at highest risk, from severe illness and death. Currently, the Pfizer vaccine is the only option currently authorized for children,” says Vanessa Slots, MD, a pediatrician with Renown Children’s. “It was found to give kids strong protection against COVID-19, including against the Delta variant. Children who are vaccinated may have some side effects (chills, redness and swelling at site injection), which are normal signs that their body is building protection.” Children are advised not to receive the vaccine if: • They are ill at the time of vaccination (fever, shortness of breath, vomiting, diarrhea or acute illness). • They have been diagnosed with COVID-19 in the previous 14 days. • They have a history of significant allergic reaction to any of the ingredients in the vaccine. About Renown Health Renown Health is the region’s largest not-for-profit integrated healthcare network serving Nevada, Lake Tahoe and northeast California. With a diverse workforce of more than 7,000 employees, Renown has fostered a longstanding culture of excellence, determination and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group and urgent care network, and the region’s largest, locally owned not-for-profit insurance company, Hometown Health. Renown is currently enrolling participants in the world’s largest community-based genetic population health study, the Healthy Nevada Project®. For more information, visit renown.org.
Read More About The Greatest Gift of All? A Fully Vaccinated Family!
-
Renown Home to "Communications Team of the Year"
Renown Health team recognized nationally for excellence in health care communications and outreach. Each year, Ragan Communications and PR Daily celebrate the most successful teams in the communication, public relations, marketing and employee wellbeing industries. As the leading voice in organizational communications – both internal and external – Ragan Communications recognizes the industry’s best communications teams. This prestigious award recognizes professional excellence while inspiring and engaging other current and future communicators regarding best practices. This year, Ragan Communications and PR Daily have selected the Marketing, Communications, Patient Experience and Community Outreach Team for Renown Health as “Communications Team of the Year.” In selecting Renown Health for this honor, Ragan judges noted that Renown Health earned its spot as a “Communications Team of the Year” for their communications response to the COVID-19 pandemic and for engaging the community to build a high-quality, trusted and desired health care experience, brand and reputation. Specifically the judged noted that Renown “implemented a Health Incident Command Structure to serve the community, organizing communications resources to mitigate, prepare, respond, communicate and recover from the COVID-19 outbreak and enhancing Renown ‘s capacity to provide access to care. The Renown team also implemented a plan to communicate safety, and prevention messaging, creating and distributing timely, accurate, and relevant communications customized to audience needs to reduce anxiety and maintain Renown’s leadership position for patient safety.” Judges also noted the success of the inspirational brand and messages of the “Fight the Good Fight” campaign, which helped to inspire and motivate a community through a difficult time. Through the pandemic, the Communications team also successfully implemented a new website, renown.org. Over 2.2 million people a year now visit the site to find a doctor by reading honest reviews from certified patients for Renown Medical Group providers, enroll for Hometown Health insurance benefits or seek health information or care. The Renown Health Marketing, Communications, Patient Experience and Community Outreach Team is led by Suzanne Hendery, Cristal Herrera, Emily MacMillan, Whitney Hansen and Annie Zucker and represent professionals with research, digital, web, communications, marketing, outreach, customer service and relationship-building expertise. The team was selected as one of three health care organizations and amid a flood of impressive entrants from all industries including Twitter and 3M. Commenting on the team, Thomas Graf, MD, FAAFP, CEO of Renown Health said, “We are very proud that Renown Health has been honored for excellence in communications. Improving the health and wellness of an entire population of people is a huge task- and it takes all of us, working together, to accomplish great things. We focus on preventing illnesses, and we benefit from a team of professional communicators who believe in- and demonstrate our mission- to keep people healthy, to make healthcare more accessible and affordable, and to achieve the vision of a healthy Nevada.” Renown Health is hiring key roles to support the health and well-being of our community, and encourages those with a passion for service to join the Renown family to Fight the Good Fight. Apply at careers.renown.org. About Renown Health Renown Health is the region’s largest, locally governed, not-for-profit integrated healthcare network serving Nevada, Lake Tahoe and northeast California. With a diverse workforce of more than 7,000 employees, Renown has fostered a longstanding culture of excellence, determination and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group and urgent care network, and the region’s largest, locally owned not-for-profit insurance company, Hometown Health. Renown is currently enrolling participants in the world’s largest community-based genetic population health study, the Healthy Nevada Project®.
Read More About Renown Home to "Communications Team of the Year"
-
New Renown Health Scholarship Supports UNR Med Students - The Next Generation of Physicians and Health Care Professionals
Clinical affiliation to create more access to care for Nevadans. View the original press release by the University of Nevada, Reno School of Medicine. Nevada continues to face a physician shortage ranking No. 45 in the United States for active physicians per 100,000 population and No. 48 for primary care physicians per 100,000 population according to the Association of American Medical Colleges (AAMC) 2019 Nevada Physician Workforce Profile. A new clinical affiliation between the University of Nevada, Reno School of Medicine (UNR Med) and Renown Health addresses the provider gap and increases access to care by developing new and innovative ways to train and retain the next generation of Nevada's health care professionals. A cornerstone of the affiliation is the Renown Health Scholarship, which was established by Renown to support UNR Med medical students and physician assistant students in their pursuit of a career in health care. The goal of the scholarship is to award $350,000 annually based on need and merit. In 2021-2022, the scholarship will be awarded to 20 first-year and third-year medical students, each receiving $15,000 for a total of $300,000; and five second-year physician assistant studies program students, each receiving $10,000 for a total of $50,000. "Students are at the core of what we do as a School of Medicine, and this incredibly generous scholarship is the best way possible for Renown Health to celebrate our partnership and support our students," says Melissa Piasecki, acting dean of UNR Med, a role that includes Chief Academic Officer at Renown Health. "We thank Renown Health for this gift that will benefit so many of UNR Med students on their journeys to becoming great doctors and physician assistants. "We are extremely proud to establish the Renown Health Scholarship with UNR Med providing annual support to students pursuing careers in health care," says Anthony D. Slonim, MD, DrPH, President & CEO, Renown Health." As Nevada's first integrated health care system, UNR Med and Renown are advancing health and health care through world-class medical education, clinical research and patient care for our community, our state and our nation, and supporting this first class of scholarship recipients is an important step in ensuring quality access to care for northern Nevada and the state in the future." The inaugural group of scholarship recipients epitomize Renown Health's and UNR Med's combined vision of A Healthy Nevada and mission of improving the health and well-being of the communities they serve. The students chosen for this scholarship further represent UNR Med's commitments to excellence and to a culture of diversity and inclusion in support of their goals of becoming physicians and physician assistants. "This scholarship will contribute greatly to my becoming a physician that can later serve those from lower socioeconomic statuses. I am humbled and honored by the fact that Renown believes that my hard work and determination are worth rewarding, I know it will alleviate some of the mental stress that finances play in my life, and I hope to make these funds count through hard work and dedication to my studies," says Eunice Aiyuk, first-year medical student at UNR Med, who was born in Yaounde, Cameroon, in West Africa, and has lived in Reno since she was three years old. Aiyuk graduated from McQueen High School and from the University of Nevada, Reno with a bachelor of science degree in neuroscience in 2018. Sergio Trejo, Jr., MPH, is a third-year medical student who grew up in Las Vegas and served as a Spanish interpreter at a community health center prior to earning his Master of Public Health degree from the University of Nevada, Reno in 2019, which instilled in him his desire to pursue a career as a primary care physician in pediatrics. "I'm interested in a career in pediatrics since I can combine my knowledge of medicine and public health to not only influence the health of children, but also the entire family, as they are ones that ultimately dictate their child's health outcomes," Trejo says. "This scholarship means the ability to fund my dream of helping alleviate health disparities in underserved communities, especially those who endure language barriers. It will help reduce the stress of funding resources that will help me be successful in my clerkships and beyond." As a second-year Physician Assistant Studies Program student at UNR Med, Benjamin "Benjie" Portillo-Dominguez's path to becoming a physician assistant started at a young age when he attended his parents' doctors' appointments so that he could interpret. He recalls his family's excitement when a health care provider could speak Spanish. "It made a world of difference because it maximized communication and helped them receive the care they needed. This helped develop in me a strong desire to pursue a career in health care, says Portillo-Dominguez, who graduated from the University with a bachelor of science degree in community health sciences in 2018. "In less than a year I will become a Physician Assistant. This has been a long-time goal of mine, but as a first-generation college graduate, this has been the dream of my parents since I was born." "Receiving this scholarship benefits me in my training because it allows me more time to focus on my studies and opens up opportunities to learn from experienced providers. Becoming the best provider I can be, allows me to strengthen this community that I was born and raised in. Having this unique perspective and being in this program allows me to be a solution to the lack of primary care providers in this area, especially with those who speak Spanish." The UNR Med student recipients of the 2021 Renown Health Scholarship were based on merit and need. They include: first-year medical students Eunice Aiyuk, Dakota Johnson, Aisha Masud, Isabella Rodriguez and Raquel Wescott; third-year medical students Davison Beenfeldt, Sara Bertram, Kaileigh Bingham, Curtis Duncan, Brooke Gantman, Alex Harper, Erin Kelley, Regina Kurapova, Ngantu Le, Otto Maurer, Keanu McMurray, Eric Nguyen, Hao To, Sean Torres and Sergio Trejo; and second-year physician assistant studies program students Ali-Marie Lostra, Margaret (Meg) Patterson, Benjamin (Benjie) Portillo-Dominguez, Preston Reugebrink and Ryan Swanson. The UNR Med/Renown Health affiliation is between a 159-year old health care provider, the state's original land grant university and the state's oldest medical school. Over the last five decades, UNR Med has educated more than 4,000 physicians with over 30% percent practicing in Nevada, increasing access to care for Nevadans across the state. Equally rooted in the community, Renown's long legacy of service started in 1862 as a county hospital, Washoe Medical Center. Now, Renown Health, a charitable, not-for-profit organization, serves the community by providing care through hospitals, outpatient medical offices, institutes and a health insurance plan, Hometown Health. Media Contact: Julie Ardito, APR Senior Director, Advancement and Engagement Email: news@med.unr.edu Office: 775-784-6006 About The University of Nevada, Reno School of Medicine The University of Nevada, Reno School of Medicine, Nevada's first public medical school, is a community-based, research-intensive medical school with a statewide vision for a healthy Nevada. Established in 1969, UNR Med is improving the health and well-being of all Nevadans and their communities through excellence in student education, postgraduate training and clinical care, research with local, national and global impact and a culture of diversity and inclusion.
-
More Space, Technology and Opportunities for Clinical Training: Renown Health, UNR and Helmsley Charitable Trust Announce the Opening of the Helmsley Simulation Center
By integrating advanced simulation technology into medical education, doctors, nurses and future healthcare providers can practice complex medical scenarios in a safe, controlled environment- ultimately improving patient safety and teamwork. Renown Health announces the opening of The Helmsley Simulation Center, a training facility designed to enhance healthcare education and clinical excellence across northern Nevada. “The opening of The Helmsley Simulation Center marks a significant milestone in our commitment to advance clinical training for area healthcare professionals across the state of Nevada,” said Brian Erling, MD, MBA President & CEO, Renown Health. “This state-of-the-art facility builds the confidence and skills of current and future healthcare professionals with hands-on, real-world training to enhance patient care and outcomes. As a not-for-profit organization, Renown relies on fundraising support. We are grateful to the Helmsley Charitable Trust for their partnership and generous support in making this vision a reality.” The Helmsley Simulation Center represents a significant collaboration between Renown Health and The Leona M. and Harry B. Helmsley Charitable Trust, which granted Renown Health Foundation $3.1 million in 2022 to construct this innovative facility. The grant supports one of Helmsley’s core program areas; strengthening rural healthcare. “Simulation education has become standard practice for many of our healthcare personnel,” said Erin Van Kirk MSN, RN, Director of Nursing Education, Renown Health. “This simulation lab will provide expanded opportunities in a controlled setting where physicians, nurses, and students can gain valuable experience in providing the best care possible.” “This center does much to support Renown Health’s strong and important partnership as an academic health system with the University of Nevada, Reno School of Medicine, and the Orvis School of Medicine, where we are working to expand training modules focused on rural health, virtual care and telemedicine for our medical students and learners,” said Paul Hauptman, MD, Dean, UNR Med and Chief Academic Officer, Renown Health. “This is a remarkable resource that bridges academic excellence with clinical practice- and it is a dream come true for me and those I work with and teach,” said Kirk Bronander, MD, an academic hospitalist at Renown Regional Medical Center and Director of Simulation at UNR Med. “For decades, airlines have relied on simulation training to ensure pilots are prepared for any situation. Now, we are bringing that same level of rigor and hands-on experience to healthcare. By integrating advanced simulation technology into medical education, doctors, nurses and future healthcare providers can practice complex medical scenarios in a safe, controlled environment- ultimately improving patient safety, decision-making and clinical outcomes. This is particularly crucial for clinicians serving in our rural and underserved areas.” “Our mission is to ensure that healthcare providers in all communities have access to high-quality training and resources,” said Wayne Booze, Rural Healthcare Program Director. “By supporting Renown Health, we are investing in the future of healthcare across Nevada and empowering providers to deliver life-saving care. The Center fits with our goal to level the playing field by giving rural residents and providers access to top-notch healthcare, regardless of their ZIP code. The new center will enable Renown Health to train substantially more nurses, physicians, community clinical partners, medical students and rural providers while improving medical and nursing expertise to support staff throughout northern Nevada.” Features include real-life acute, outpatient, telemedicine and specialty care scenarios with; Six patient rooms designed to simulate real-world clinical environments, including acute, outpatient, telemedicine and specialty care settings; Four advanced simulation “people and baby” manikins, capable of mimicking a wide range of medical conditions and responses; Advanced equipment includes a telemetry monitor, IV and epidural equipment, a code cart, a defibrillator, a balloon pump, ventilators and a cooling machine; Two debriefing rooms, where educators can review scenarios with participants, analyze decision-making processes and provide constructive feedback. “Our mission as a health system and Nevada’s first hospital is to serve our community as the only not-for-profit academic health system, committed to saving lives, nurturing minds, and caring for all people,” said Melodie Osborn, MBA, BSN, RN, Chief Nursing Executive and sponsor of the project. “Opening the simulation center, you feel our mission in action. The simulation center will serve a wide range of learners including nurses, physicians, community clinical partners, EMTs and first-responders, medical students and rural providers. This state-of-the-art simulation center expands our academic partnerships and substantially increases training capacity from 1,500 to 2,500 clinicians each year across urban and rural settings. In addition, we will foster confidence, teamwork and clinical expertise with the care teams that care for almost a million patients and their families. It’s a very exciting and important day.” Yesterday, Becker’s Healthcare listed The Helmsley Simulation Center at Renown Health as one of the nation’s 64 Simulation and Education Programs to Know. "I am proud that northern Nevada and Renown Health, with support from The Helmsley Charitable Trust, are investing in the future of healthcare for our region,” said Greg Walaitis, MBA, Renown Health Foundation Chief Development Officer. “Delivering best-in-class care begins with ensuring every provider, whether new or experienced, has access to a space where they can continually refine and enhance their skills. This generous grant for the new simulation center from The Helmsley Charitable Trust is truly an investment in the bright future we envision for Renown, our care teams and the community.” About Renown Health Renown Health is the region’s largest locally governed, not-for-profit integrated academic healthcare network serving Nevada, Lake Tahoe and northeast California. With a diverse workforce of more than 7,500 employees, Renown has fostered a longstanding culture of excellence, determination and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group and urgent care network and the locally owned not-for-profit insurance company, Hometown Health. For more information, visit renown.org. About The Helmsley Charitable Trust The Leona M. and Harry B. Helmsley Charitable Trust aspires to improve lives by supporting exceptional efforts in the U.S. and around the world in health and select place-based initiatives. Since beginning active grantmaking in 2008, Helmsley has committed more than $4.5 billion for a wide range of charitable purposes. Helmsley’s Rural Healthcare Program funds innovative projects that use information technologies to connect rural patients to emergency medical care, bring the latest medical therapies to patients in remote areas, and provide state-of-the-art training for rural hospitals and EMS personnel. To date, this program has awarded more than $750 million to organizations and initiatives in the states of Hawaii, Iowa, Minnesota, Montana, Nebraska, Nevada, North Dakota, South Dakota, Wyoming, and two U.S. Pacific territories, American Samoa and the Commonwealth of the Northern Mariana Islands. For more information, visit www.helmsleytrust.org.
-
56 Anesthesiologists Join Renown Health to Provide High Quality Services to Area Patients and Surgeons
Innovative anesthesiology practice improves diagnosis, medical management and quality of life for patient. If you are preparing for a surgical procedure, you have probably given a lot of thought to the education, training and experience of the surgeon performing the procedure. But you may not have thought much about the physician anesthesiologist or the importance of his or her medical expertise in your procedure — before, during and after — to keep you safe and comfortable. "Our leadership team has thought a lot about physician anesthesiologists over the past year,” says Sy Johnson, MBA, President and Chief of Staff for Renown Health. “As the region’s only not-for-profit integrated healthcare network and trauma center, we are trusted and chosen by patients as the top provider of inpatient care, including surgeries, for northern Nevada, Lake Tahoe and northeast California. To serve the needs of hundreds of surgeons and thousands of patients with safe, high quality and effective anesthesia coverage, we now employ fifty-six anesthesiologists through our Department of Surgery and have established Renown Medical Group Anesthesiology, a new local practice for northern Nevada.” “Renown Medical Group anesthesiologists provide 24 hour surgical and procedural coverage based on clinical skill sets, surgeon preference and patient preference. Patients who choose Renown for their care can feel certain that they are receiving anesthesia care from a physician anesthesiologist who has attained board certification. Renown Health hospitals are pleased to provide patient care exclusively by physician anesthesiologists,” says Thomas Graf, MD, FAAFP, CEO, Chief Clinical & Quality Officer of Renown Health and Senior Associate Dean for Clinical Affairs at the University of Nevada, Reno School of Medicine. “We are the doctors trained to administer and manage anesthesia given to a patient during a surgical procedure to ensure anesthesia care is as safe and effective as possible,” says Nariman Rahimzadeh, MD. Dr. Rahimzadeh serves as Medical Director and Chief of Staff for Renown South Meadows Medical Center, is a member of the new group and has practiced in Reno for fifteen years. “We also play a key role in taking care of patients who are having minor surgery or who may not require general anesthesia, such as women in labor who need to be awake and alert but require effective pain management.” “Our innovative anesthesiology practice is now staffed by fifty-six anesthesiologists. We are serving patients and surgeons at Renown Health hospitals with one fully integrated model of care to improve diagnosis, medical management and quality of life,” says Christos Galanopoulos, MD, MBA, MSc, FACS; Chair, Department of Surgery and Vice President at Renown Health. “We strive to advance anesthesia through clinical excellence, education, innovation and people. Our nationally recognized medical staff and dedicated support team perform the majority of anesthesia procedures in our market, and evaluate, monitor, and supervise patient care before, during, and after surgery to deliver effective anesthesia and ensure optimal patient safety.” “Physician anesthesiologists have 12 to 14 years of education, including medical school, and 12,000 to 16,000 hours of clinical training,” adds Scott Parkhill, MD, FASA, who serves as a Medical Director and Vice Chief of Staff at Renown Regional Medical Center and is a member of the new group. “Physician anesthesiologists in the United States complete a four-year undergraduate college degree that includes satisfying pre-med requirements. Like other medical doctors, they must follow undergraduate education with four years of medical school. After medical school, a physician specializing in anesthesiology completes a four-year anesthesiology residency program. Following completion of a residency program, residents are eligible to sit for the American Board of Anesthesiology (ABA) exam. We are pleased that all of our Renown Medical Group anesthesiologists are board certified.” Adds Kelsey Larsen, MBA, Chief Operating Officer for Renown Medical Group, “We are thrilled to welcome and employ forty-two physician anesthesiologists who started with us on April 1. An additional nine physicians joined last week and five other physicians have requested to start over the summer for a total of 56 anesthesiologists that have joined Renown Health to provide services to patients.” Patients served include those at Renown Regional Medical Center, the only Level II Trauma Center between Sacramento and Salt Lake City, and named #1 Hospital in the State of Nevada by U.S. News and World Report Best Hospital Rankings for 2021. Physician anesthesiologists will also provide services to patients at Renown South Meadows Medical Center, named #1 Best Hospital for 2020 by U.S. News & World Report; and to patients at Renown Rehabilitation Hospital, northern Nevada’s only Commission on Accreditation of Rehabilitation Facilities (CARF) accredited hospital, specializing in the treatment of patients with brain injury, spinal cord injury and stroke. Renown Health is integrated with the University of Nevada, Reno School of Medicine, Nevada’s first medical school, which serves to enhance the health of the community through increased access to care, innovative health care delivery, expansion of clinical research and training for the next generation of physicians and health care professionals. 51 ANESTHESIOLOGISTS WHO JOINED RENOWN IN APRIL 2022: Samuel Beck, MD Heber Becker, MD Peter Billharz, MD Kara Bjur, MD Brian Brewer, MD Brian Buehler, MD Carrie Buehler, MD Catherine Burton, MD Joshua Cartinella, MD Nicholas Cirac, MD Gordon Curry, MD Scott Dougan, MD JoAnn Ellero, MD Daryl Fenio, MD Dirk Fletcher, MD Tobey Gansert, MD Benjamin Garol, MD Jeffery Grudzinski, MD Keith Hanson, MD Min Hein, MD Mark Janes, MD Scott Jeannes, MD Kevin Lasko, MD Sarah Lim, MD Jay Markin, MD John Marshall, MD Eric Moody, MD John Mortensen, MD Jobin Nash, MD Mel Nutter, DO Scott Parkhill, MD Nariman Rahimzadeh, MD Suresh Raman, MD Shaina Richardson, MD Alan Sarabia, MD Heidi Sarabia, MD Mitch Seman, MD Daniel Sorensen, MD Ryan Stites, MD Aaron Wallace, MD Duncan Browne, MD Tyler Hartley, MD Jie Lan, MD Pamela Russell, MD Scott Reineck, MD Brian Landreth, DO Kara Sievert, MD Chiaki Nakanishi, MD Philip Phu, MD Matthew Sabatini, MD Robert Kyper, MD About Renown Health Renown Health is the region’s largest, locally governed, not-for-profit integrated healthcare network serving Nevada, Lake Tahoe and northeast California. With a diverse workforce of more than 7,000 employees, Renown has fostered a longstanding culture of excellence, determination and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group and urgent care network, and the region’s largest, locally owned not-for-profit insurance company, Hometown Health. Renown is currently enrolling participants in the world’s largest community-based genetic population health study, the Healthy Nevada Project®. For more information, visit renown.org
-
Nationally Recognized Vascular Surgeons Join Renown Health
Two vascular surgeons bring a quarter of a century of experience to patients and community. As part of a continuing focus to bring comprehensive care to patients experiencing cardiac and vascular disease across northern Nevada, Renown Health Department of Surgery and Renown Institute for Heart & Vascular announce that vascular surgeons, John C. Hansen, MD, FACS and Benjamin P. Jaquish, MD, FACS have joined Renown Health. "Recognizing the significance of preventing, diagnosing and caring for people with heart and vascular disease, which continues to be on the rise and taking far too many lives, is of critical important to us at Renown," says Christos A. Galanopoulos, MD, MBA, MSc, FACS, VP, Chairman Department of Surgery at Renown Health. "Both Drs. Hansen and Jaquish are superb clinicians, skilled investigators, and effective educators. We are fortunate to have them helping to lead the growth of both the department and the Division of Vascular and Endovascular Surgery." Together, the vascular surgeons have more than 26 years of combined experience caring for northern Nevadans. Dr. Hansen has 20 years of experience in northern Nevada. He is a clinical associate professor of surgery at the University of Nevada, Reno School of Medicine (UNR Med) and currently serves as medical director of vascular and endovascular surgery for Renown Regional Medical Center. "Since 2002, Dr. Hansen has led our region with his expertise and knowledge of aortic stents, grafting for abdominal aortic aneurysms and thoracic aneurysms, as well as treating patients with carotid disease," says Jayson Morgan, MD, FACC, Director, Cardiovascular Services. "Dr. Hansen specializes in the comprehensive management of vascular disorders, including open and endovascular surgeries. He is meticulous, thorough, and compassionate in the extraordinary care he provides to patients. We are thrilled that he has joined the Institute for Heart & Vascular Health team at Renown." Dr. Hansen completed his fellowship in Vascular Surgery at the Mayo Clinic in Rochester, MN, and completed his residency in General Surgery at the University of South Carolina, Greenville. He graduated with his Doctor of Medicine from the University of North Carolina School of Medicine, Chapel Hill, and is board certified in both Surgery and Vascular Surgery from the American Board of Surgery and a Fellow of the American College of Surgeons. Dr. Hansen has an interest in complex and acute vascular surgery and is committed to expanding access to qualified vascular care in the region. His mission is to further develop and establish Renown as a premier vascular center in northern Nevada. "Dr. Jaquish has extensive experience in carotid artery disease, carotid endarterectomy, aortic aneurysm and dissection, and peripheral vascular disease," says Sam Obilie-Mante, MBA, MIS, RDCS, RVT, LBBP, VP Administrator, Cardiovascular Services. "Dr. Jaquish is intelligent, professional, conscientious, and always perseveres on behalf of his patients. How proud we are to have him bringing his time and talent to patients across Renown Health." Dr. Jaquish received both his B.S. in Biochemistry (2005), graduating Magna Cum Laude with his Doctor of Medicine (2009) from the University of Nevada, Reno School of Medicine. Dr. Jaquish completed his fellowship in General Surgery at Ascension St. John Hospital and Medical Center in Detroit and a fellowship in Vascular Surgery at Texas A&M at Baylor, Scott & White Hospitals in Temple, TX. He is board certified in both General Surgery and Vascular Surgery. Dr. Jaquish currently serves as Assistant Professor of Clinical Surgery for UNR Med. Dr. Jaquish is bilingual in Spanish, proficient in American Sign Language and serves as an instructor for Advanced Trauma Life Support. Why Vascular and Endovascular Care Matters to You People with complex and serious conditions of the blood vessels and lymph system (vascular diseases) often find the help they need from Renown Health's vascular and endovascular surgical team. Renown's experts provide coordinated and comprehensive treatment to people of all ages. Renown's surgeons use advanced technology to perform vascular and endovascular surgery, including complex stenting procedures, blood clot removal and bypass surgery. Conditions treated include peripheral artery disease, aortic disease, mesenteric disease, nutcracker syndrome and carotid artery disease. "Our expert vascular and endovascular surgeons and staff treat problems that extend from mild to the most critical of emergencies," says Adnan Akbar, MD, Chief Medical Officer for Renown Acute Care. "Specialized physicians including cardiologists, interventional radiologists, heart and vascular surgeons, emergency medicine and trauma surgeons, neurologists, radiologists, physical medicine and rehabilitation specialists, primary care providers, nurses and other clinicians work as a team to determine the best treatment plan for each patient. We encourage all patients to discuss with their primary care providers whether they should undergo formal screening for early vascular disease." "Renown's reputation as the region's vascular and endovascular care leader has been built over many years. We performed the area's first open-heart surgery, angioplasty, stent and valve replacements decades ago. Renown Regional offers incredible advancements like trans-catheter aortic valve replacement (TAVR) and trans-catheter mitral valve repair (TMVr) with MitraClip therapy, lifesaving alternatives to open-heart surgery for patients considered high-risk or inoperable," says Chris Nicholas, FACHE, Chief Executive Officer of Renown Regional Medical Center. "Offering the highest level of comprehensive care for patients experiencing cardiac and vascular disease, Renown developed its first division of cardiothoracic surgery dedicated to heart surgery patients in 2019." The Renown Institute for Heart & Vascular Health program now offers a Diagnostic Electrophysiology Lab; a Chest Pain Center using the D-SPECT® heart camera; multiple Interventional Labs; Heart Failure Program; several Cardiac Catheterization Labs; Interventional Cardiology and Cardiac Surgery when necessary; and the only Pritikin-certified Healthy Heart Program in the West, creating individualized rehabilitation plans tailored to each patient's needs, so they can exercise safely, eat healthy, manage stress and cook nourishing, balanced meals, all while gaining a healthy mindset. In the most recent US News & World Report Best Hospital rankings, Renown Regional Medical Center was named as the number one hospital in Nevada. No other hospitals in the state met their stringent standards for the 2021 rankings. Renown Health is High Performing, its highest rating possible, in eight procedures and conditions including Heart Failure, Colon Cancer Surgery and Chronic Obstructive Pulmonary Disease, Hip Replacement and Knee Replacement. A hospital's score is based on multiple data categories, including patient outcomes, safety and volumes. Hospitals earning a High Performing rating were significantly better than the national average. The 2021-22 Best Hospitals rankings are drawn from a universe of 4,523 facilities, representing nearly all U.S. hospitals providing inpatient care. Hospitals are evaluated across a wide range of conditions and procedures, including 16 medical specialty areas of care. US News & World Report evaluated 58 hospitals in Nevada. Renown Health is Nevada's largest, not-for-profit integrated healthcare network serving Nevada, Lake Tahoe, and northeast California. With a diverse workforce of more than 6,500 employees, Renown has fostered a longstanding culture of excellence, determination, and innovation. The organization comprises a trauma center, two acute care hospitals, a children's hospital, a rehabilitation hospital, a medical group and urgent care network, and the locally owned not-for-profit insurance company, Hometown Health. Renown is currently enrolling participants in a community-based genetic population health study, the Healthy Nevada Project®. For more information, visit renown.org. The University of Nevada, Reno School of Medicine (UNR Med), Nevada's first public medical school, is a community-based, research-intensive medical school with a statewide vision for a healthy Nevada. Since 1969, UNR Med has trained more than 3,900 students, residents and fellows. UNR Med continues to improve the health and well-being of all Nevadans and their communities through excellence in student education, postgraduate training and clinical care, research with local, national and global impact and a culture of diversity and inclusion. For more information, visit med.unr.edu.
Read More About Nationally Recognized Vascular Surgeons Join Renown Health
-
Get Moving: How to Exercise with Arthritis
An arthritis diagnosis doesn’t mean your exercise routine has to end. In fact, a consistent routine can actually improve mobility. Although stiff and painful joints can make it difficult to keep moving, staying active is essential for easing pain. October 11 is World Arthritis Day, so we asked Michelle Higgins, MPT at Renown Physical Therapy & Rehab some advice about exercising with arthritis. According to the Arthritis Foundation, arthritis affects one in five adults and 300,000 children. As a matter of fact arthritis is the nation’s leading cause of disability. Your joints certainly don’t need to suffer when you exercise. In general exercise is actually necessary for those with arthritis. Not only does it reduce joint pain, but it also increases strength and flexibility. Furthermore those adopting a regular exercise routine also have more energy, deeper sleep and find it easier to maintain a healthy weight. “Exercise is a necessary component to managing your arthritis,” says Higgins. “Consistent participation in an exercise program has been shown to promote long-term pain relief, increased body function and an improved quality of life. Alternatively, a lack of exercise can actually increase joint pain or stiffness and eventually lead to long term disability and suffering.” Exercising With Arthritis Exercise truly is the most effective non-drug arthritis treatment available for reducing pain and improving movement. And it can even include daily activities like gardening, dancing or walking your dog. Of course talk to your doctor or physical therapist about what exercises fit into your specific treatment plan. With this is mind, the four specific components below are important to an effective arthritis exercise program: Range of motion Moving joints through their full available range of movement is important. This frequently increases function and decreases joint stiffness and pain. For this reason, aim to complete these exercises daily. Examples include bending, straightening, and rotating specific joints, or static and dynamic stretching. Strengthening These exercises target muscles supporting and protecting our joints and bones. Strengthening is also necessary for weight control, so two-to-three sessions per week are recommended. In order to allow your body to adapt, begin with light resistance and start slow. Strength exercises include weightlifting and using resistance bands. Low-impact aerobic exercise Aerobic exercise is certainly necessary for overall well-being, weight management and heart health. Aim for two-to-three sessions a week. Low-impact exercises include walking, swimming, cycling, elliptical machine exercises and water aerobics. Balance Good balance is also vital for an effective arthritis program. On the positive side, solid balance prevents falls by increasing your ability to stay upright whether you are moving or sitting still. Likewise, it improves your confidence with walking and daily activities. In order to keep excellent balance, incorporate daily balance exercises. Examples of balance exercises include the use of an exercise ball, Tai Chi and exercises such as standing on one foot. Start Slow, Finish Strong As you begin your exercise program, remember to listen to your body. Start slowly – it can take several weeks for your body to adjust to exercise. Consult your doctor, or physical therapist, if you experience increasing pain or swelling which doesn’t go away with rest. Above all, incorporate fun and motivating activities so you’ll stick to them long term and improve your results. Renown Physical Therapy & Rehab 775-982-5001 Through outpatient physical, occupational and speech therapy, Renown Physical Therapy & Rehab gives you hands-on, individualized treatment in convenient Reno/Sparks locations. We have the latest, most advanced physical therapy and rehab equipment, specialty services and treatments. Renown Physical Therapy & Rehab is now open on Robb Drive in addition to three additional locations in Reno and Sparks. Call 775-982-5001 or visit us online.
-
Reno Widow Inspires New Visitor Policy for Renown
Renown Health is one of the country’s first health systems to lift visitor restrictions for patients with COVID-19 and encourage the family to be at the patient’s bedside. Read Darlene and Dave’s story to understand why we’re updating our visitor policy. Dave and Darlene Randolph found joy in exploring antique shops and garage sales to find damaged or discarded vintage pieces. Dave would spend many hours scraping, cleaning, sanding, and refinishing items, transforming them into functional, beautiful pieces of furniture. Every piece in their home rekindles a memory and has a story to tell. On Thanksgiving, when Dave was too ill to gather around their antique dining room table, Darlene called the ambulance. Ailing with COVID-19 for two weeks, Dave had not been improving. When the EMTs reached her home and asked Darlene what underlying conditions he had, she said, “all of them.” David was seriously ill. Hospitalized for COVID-19, their communications options were limited. The only way Darlene could communicate with Dave was on a video call or by telephone. Dave spent 17 days hospitalized at Renown Regional Medical Center in Reno. Darlene spent 17 days waiting by the phone for more information on his condition. Darlene said he had “up days and down days,” but thought he might be home, sitting at their antique dinner table for Christmas. Sadly, Dr. David Randolph lost his battle with COVID-19 on December 13, 2020, and died as he slept in a hospital bed. When Darlene wrote his obituary for the newspaper, she gave thanks to the “tremendous nurses and doctors at Renown Regional Medical Center, for providing his care during a time when the family could not be with him.” Taking Action to Inspire Change Darlene wished she could have been there. Over their 45-year marriage, she had always been there. Darlene said, “I had always been at his bedside, as his advocate, to help communicate and straighten things out.” As a registered dietician, she worked in hospitals, knew the protocol, and knew that Renown had a restricted visitor policy to stop the virus’s spread- to other patients, staff, and their family members. Still, she wished she could have spent more time with him. On Christmas Eve, she sat down and wrote to Renown leadership. “As the wife of a COVID patient who recently passed away in your hospital, I want to express my thanks to you and your staff for the care he received in the last days of his life. I am aware that the nurses and staff are working under dangerous conditions and risking their health and lives by caring for multiple COVID patients. The staff is gracious, concerned, and doing everything they can.” She continued, “I know procedures are changing every hour to try to stay ahead of this dangerous virus, and I am sharing my experiences, hoping they will be helpful when establishing policies that impact families.” Darlene explained that despite receiving assurances that Dave’s nurse or a doctor would call daily, sometimes they would forget. She explains in her letter, “how important it is, in these times when the family cannot visit, and has only infrequent communication and is anxiously waiting at home for information about their loved one, how much it means to get a call from someone caring for him at the hospital. If there is a way you can help assure nurses have time to make calls or assist patients in making calls because it is an important part of patient care.” A Person-Centered Visitor Policy After receiving her letter, Renown leadership called Mrs. David Randolph to thank her, offer his sympathies and ask if Renown could help in any way. Darlene asked if he might reconsider allowing families to visit hospital patients during treatment for COVID-19. As the COVID-19 situation has evolved, the policy has as well. Renown hospitals and medical practices now encourage limited visitors for all patients, including those diagnosed with COVID-19. Renown also has extra safety measures to protect the health of patients, visitors and healthcare employees. Darlene is very pleased that her letter inspired this shift in visitor policies for patients with COVID-19. She says, “I have always tried to think of ways I could help other families. Especially those senior couples where one has been hospitalized and the other is home. My wish is to help others.” Renown Health Visitor Policy Renown Health patients may identify two healthy adult “patient supporters” to accompany them on their hospital stay. For more details, visit our Patient Supporter Guidelines page.
Read More About Reno Widow Inspires New Visitor Policy for Renown
-
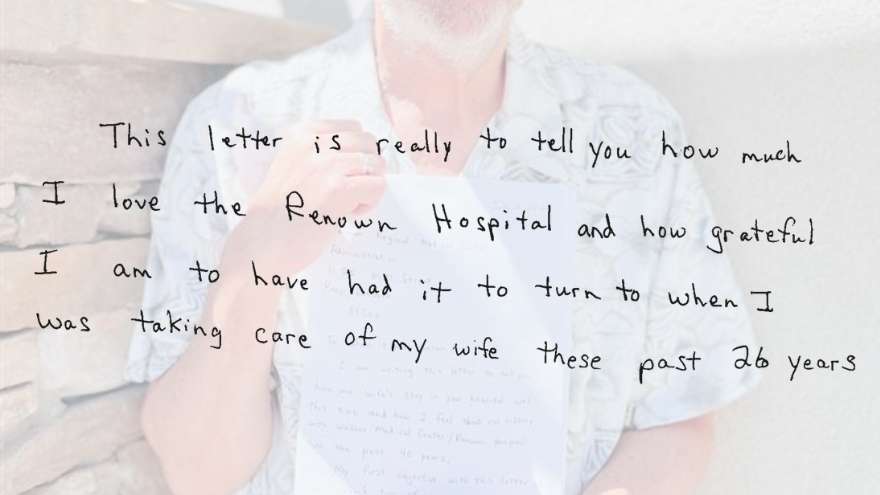
40 Years of Exceptional Care
“In sickness and in health” are words we often hear when celebrating the momentous occasion of marriage with our friends, families and loved ones. For James Breckenridge, these words were the foundation of the love and commitment he and his wife Carolyn showed to each other during their 30 years of marriage. In health, James and Carolyn shared a love of traveling. Hopping in their van, driving across the continental United States and enjoying the views along the way will be a memory James cherishes forever. Unfortunately, their excursions would be cut short when Carolyn fell ill, rerouting to their local hospital, Renown Health. Carolyn has spent more time at the hospital than the average person – including recovering from COVID-19 at Renown South Meadows Medical Center. However, hospital admittance for Carolyn meant the same for James, providing support to his wife during her stay. Following more than 40 years of exceptional experiences with Renown and their most recent discharge from the hospital, James wrote a letter recognizing the efforts of the team members and healthcare providers who not only cared for Carolyn but also James. To Whom It May Concern James began his letter by applauding two Renown Regional nurses they got to know well during their recent visit. Tiffany and Ashley went the extra mile to care for Carolyn attentively. From simple tasks like gathering requested supplies to answering James’ questions in detail, they helped provide a comfortable environment for the couple. To these nurses, these tasks may have felt like another day at work. Still, James’ letter commends them for their acts of service, reminding us that every interaction we have with a patient can be a memorable one. Tiffany and Ashley weren’t the only team members who received recognition in James’ testimonial. He also took a moment to recognize the various nurses, certified nursing assistants, therapists and doctors they encountered during their care journey. All provided the excellent and helpful experience we aim for at Renown. Healing Memories James first brought Carolyn to Renown Regional Medical Center, formerly known as Washoe Medical Center, in 1980, but it was 1996 when things changed for him. Carolyn was admitted to the hospital for a procedure they originally anticipated would come with a difficult prognosis. To their surprise, doctors found the opposite. It was in that joyous moment that James’ perspective of hospitals shifted, now viewing them for what they truly are – a place people go to get better. “Every time I walk around Renown Hospital, I remember all the times Carolyn was healed there,” James wrote in the latter half of his letter. Healing Isn't Just for the Patient James took advantage of the many support resources accessible to family members during their time at Renown. These donor-funded hospital initiatives are a valuable mental health resource in difficult circumstances. Whether it was an afternoon stroll with his wife through Fianna’s Healing Garden or quiet time alone in the Spiritual Center, James never hesitated to turn to these resources in his time of need. “Although I know the Tahoe Tower is the modern, state-of-the-art part of Renown, I prefer the Sierra Tower because that is where most of my memories are.” Even a simple daily walk to the on-campus Starbucks was a notable part of his day – grabbing a cup of coffee for himself and often a treat for Carolyn. An Inspiration in Healthcare When asked to describe Renown in one word, James chose “inspirational.” His collective experiences with Renown, James said, “helped him to be a better healthcare advocate” when his wife received care at other hospitals. As a healthcare leader, we challenge ourselves to go above and beyond for the health of our entire community. Collaborating with our patients and their families is at the center of everything we do at Renown. Positive reviews mean the absolute world to us, and something about this handwritten letter feels even more special. We could not be more appreciative to James for sharing how our vision to inspire better health in our community was reflected in his 40 years of experience with Renown. We were saddened to hear of Carolyn’s passing during a recent meeting to thank James for his letter. We take solace hearing James’ beautiful memories of his wife and knowing that Renown Health was there in times of sickness and health. We offer our sincere condolences to James, Carolyn’s children and their family members.
-
Your 9-Step Guide to Prevent Falls
According to the Centers for Disease Control and Prevention (CDC), one out of three adults aged 65 or older, fall each year. But less than half of those who fall talk to their healthcare provider about it. What’s more, among older adults, falls are the leading cause of both fatal and nonfatal injuries. Senior Care Plus, a Medicare Advantage Plan by Hometown Health, and Renown Health Nurse Educator, Darlene Roberts, worked together to provide a list with simple tips to help you prevent falls. 1. Exercise Exercise strengthens both your muscles and bones and improves balance which is a key factor to preventing falls. The stronger you are, the less likely you are to fall. And, if you do fall, you are less likely to be injured. 2. Vision Check Vision is an import part of fall prevention, have your eyes check by an eye doctor at least once a year. Update your vision prescription and replace your eyeglasses as needed. 3. Install Safety Equipment in Your Bathroom Installing grab bars in your home bathroom provides a way for you to help yourself in and out of challenging situations. It also provides support if you suddenly feel week or unstable. Having a grab bar to lean on or hold onto when you feel yourself falling or slipping can help prevent falls. Rubber mats eliminate slick surfaces that increase your risk of falling. Learn more about safety and medical equipment that are available through the Care Chest of Sierra Nevada. 4. Helpful Items in Your Bedroom A light within reaching distance is an important item to have in your bedroom. One reason adults fall is because they wander through a dark room, often to get to the bathroom at night, and can’t see where they are walking. Having a light within reach that is quick and easy to turn on before walking around a room can make it safer and decrease your risk of falling. Having a bedroom that is organized and furnished in a way that is easy to navigate is also important. If your bedroom is cluttered and hard to walk around without tripping or running into things, it might be worth reorganizing the area to define a clear walking path. 5. Helpful Items in Your Living Room Similar to your bedroom, your living room should have a light that is easily accessible. Sofas with armrests are helpful for support when getting up and sitting down. Avoiding clutter in your walkways, rugs that are not secured down and unstable furniture are important to consider when preventing falls. 6. Actions to Avoid in Your Home There are other ways to fall besides slipping or tripping while walking. Never stand on chairs, boxes or other unstable items in your home. Walkways should be tidy and free of objects that you could trip on. Spills should be cleaned up right away to prevent slipping. 7. Wear Appropriate Footwear Wearing shoes with non-slip soles and closed toes can help prevent you from falling. Having shoes that fit properly, are made from hard rubber (like tennis shoes) and provide good support help prevent tripping and falling. Shoes with a collar that support the ankle and a well-padded tongue for the top of your foot can also help prevent injury to your feet. 8. Review Your Health & Medications at your Annual Health Check-Up It is important to review your health and medications with your healthcare provider so they can assess if you are at risk for falls. You should discuss your vision, heart health and blood pressure at your annual health check-up. These things can play a role in the risk of falling. Reviewing your current medications is also important. If medications are making you dizzy, talk to your provider about adjusting the dosage so you can feel more stable and balanced. When talking to your doctor about medications be sure to include your vitamins and supplements. Finally, Have your healthcare provider check your feet and discuss proper footwear yearly. Remember to speak up and talk openly with your healthcare provider about fall risk and prevention 9. Avoid Smoking and Alcohol Balance is important in preventing falls. Alcohol consumption negatively affects balance and increases your risk for falls and fractures. It also increases your risk for cancer, liver damage, osteoporosis, high blood pressure and strokes. Smoking is connected to frailty in older adults. It prevents the development of muscle tissue and breaks down healthy muscle tissue due to the lack of oxygen in your body. Stay up-to-date with resources, classes and workshops on falls prevention with UNR Med's Sanford Center for Aging.
-
Navigating Pain with Renown Spine, Sports & Pain Management
Chances are you or someone you know will deal with chronic pain at some point in life. In fact, in the U.S. alone, one in five adults have experienced chronic pain in recent years, according to the Centers for Disease Control and Prevention (CDC). The road to relief is a frequently traveled one that can be filled with twists and turns, so it’s important for patients to have a trusted provider by their side navigating that journey. We interviewed Dr. Sharlene Su, a pain management physician with Renown Medical Group, who told us what patients can expect when seeking care with Renown Spine, Sports & Pain Management (RSSPM) and all about the variety of pain relief options available to patients. What pain management treatment options are available outside of painkillers? This depends on someone’s root cause of pain. For example, for pain from arthritis of the spine or major joints, radiofrequency ablation can relieve most of the pain for six months to two years, which can be life changing. If someone is suffering from a pinched nerve in the neck or back, an epidural can be useful. Nerve stimulators can also be a great option to relieve pain for years. One of the advantages of the procedures we perform at RSSPM is that they reduce the need for painkillers, which are notorious for having side effects of their own. Physical therapy can also be a very helpful tool to treat pain. It is an exciting time in the field of pain medicine right now because new advances are -constantly being made. At Renown, we pride ourselves on staying current with the most cutting-edge treatments to ensure our patients always have the best available to them. What are some at-home tips and tricks that patients experiencing pain can do on their own for some relief? If pain is related to posture or physical activity, consider doing stretching and strengthening exercises. YouTube can be a great (and free) resource for this. In terms of medications, over the counter topical pain creams can be great. Tylenol is one of the safest pain medications for those without preexisting liver conditions. On a short-term basis, anti-inflammatory medications can often be used safely depending on one’s overall health. Ice and heat can both be useful for treating muscle pain. Can you tell us more about the services Renown Spine, Sports & Pain Management offers? Our team specializes in identifying the root cause of each patient’s pain and partnering with them to develop a custom plan tailored to their individual needs, which can involve injections, physical therapy and medications. We treat patients ranging from top-level athletes, to weekend warriors, to grandparents who’d like to be able to keep up with their grandkids. Once we relieve a patient’s pain, our role then transforms into a coach, educating and guiding our patients on how to prevent their pain from coming back. At RSSPM, you’ll see the same doctor every time, which means that your provider will get to know you very well, and you’ll receive the same high-quality consistent care whenever you come for a visit. Renown has a unique pain management team called “Special Procedures” that not many people may realize is a great option for care. How does this team treat pain? Our Special Procedures team is crucial to the high-quality pain management care that we provide. We have an amazing staff that assists with X-ray guided procedures including epidurals, radiofrequency ablations, joint injections and nerve stimulators. Dr. Casey Keating, our division chief, and I work with this team to ensure that every procedure is done with the same precision, attention to detail and quality. The Special Procedures team regularly receives feedback from patients on how well taken care of they felt during their procedure. If someone is experiencing pain from an injury or even an unknown reason, what should they do to get care for their concerns? Contact your primary care provider for a referral to have an evaluation with us! RSSPM accepts most insurance plans and are proud that our wait times are averaging less than one week to be seen as a new patient. Two more doctors will be joining us in the next few months, which should reduce our wait times even more. There are so many targeted and effective ways to treat pain nowadays, and it is worth addressing to live the life you want to live.
Read More About Navigating Pain with Renown Spine, Sports & Pain Management