Search
Results for 'social work'
Clear-
A First-Hand Account of a Renown Health Kidney Transplant Evaluation Experience
When Angela Seagraves was told she had kidney disease at the young age of 30-something, her health became even more center stage. After many unsuccessful attempts at getting care out-of-state in hopes of a transplant, the Renown Patient Access Representative would experience a “dream come true” with the establishment of the Renown Transplant Institute, Reno’s first-ever kidney transplant program. Angela tried many things to keep her kidneys in check after her diagnosis. However, getting COVID-19 four times would be what would accelerate her into stage five kidney failure by March 2023. With her kidneys operating at 12%, she began dialysis in June of that same year, going in three days a week for three hours of treatment each time. With no kidney transplant program in northern Nevada at the time, Angela was forced to look outside the area, without success. Feeling discouraged, she continued dialysis, hoping for an answer. That answer then came when she started seeing announcements on Renown’s intranet regarding the grand opening of the Renown Transplant Institute and the kidney transplant journey of Kirill Zelenin, the son Renown Clinical Application Specialist Masha Zelenin. After being referred to the Institute by her care team at DaVita Dialysis Center, Angela scheduled her evaluation appointment. Here’s a breakdown of what she experienced. Angela’s First Appointment at the Renown Transplant Institute Angela was excited to know that she would only have to wait a couple of weeks to be seen for her full-day appointment at the Renown Transplant Institute. She felt nothing but optimism when the day came. After she checked in at 7:30 a.m., her appointment started with a Transplant 101 education class, a detailed overview of the transplant process. She was then brought into the office to meet the multidisciplinary transplant team, including: Dr. Ernesto Molmenti, Executive Director of the Renown Transplant Institute and Chief of Transplantation at Renown Health Dr. Narisorn Atsava-Svate, Transplant Nephrologist for the Renown Transplant Institute Transplant nurse coordinators, a pharmacist, a dietician, a social worker and a financial coordinator Together, the team review her medical history, discussed what makes a good transplant candidate and explained the tests required as part of her evaluation. “These people were some of the kindest, most genuine people I’ve ever met,” she said. Following the team meet-and-greets, Angela was sent to the lab, where the phlebotomists took several blood samples. Then, she walked over from the lab to the imaging room, where she ended her full-day assessment with a chest X-ray and a CT scan of her abdomen and pelvis. Time of check-out: 3:30 p.m. Angela walked out of her appointment with restored hope, noting how “wonderful the support system is” at the Renown Transplant Institute.
Read More About A First-Hand Account of a Renown Health Kidney Transplant Evaluation Experience
-
5 Health Benefits of Spending Time Outside
Spending time in the great outdoors is undoubtedly beneficial for our physical and emotional health. According to the Harvard T.H. Chan School of Public Health, getting outside and experiencing “green space” is linked to a reduced risk of chronic disease or even death. Living in northern Nevada makes it easy to enjoy time outside. Reno was voted the happiest place to live by Outside Magazine in 2023, partly because of our easy access to the outdoors. In fact, Outside Magazine reported that 76% of Reno residents live within a 10-minute walk of one of our city’s 87 parks. The Nevada Division of Forestry and Nevada Division of Outdoor Recreation encourage every Nevadan to engross yourself in the beauty – and positive health effects – of nature and to enjoy time outdoors responsibly. Below are five benefits you may experience by spending at least a few minutes a day outside: 1. Improved Mental Health Being in nature helps lower the body’s stress hormone, otherwise known as cortisol levels, and increases feelings of relaxation and well-being. Whether it’s taking a walk in the park, hiking along one of northern Nevada’s many trails or simply sitting in a garden, being surrounded by green spaces has been shown to elevate mood and reduce mental fatigue. 2. Boosted Immune System Exposure to fresh air and natural environments can improve your immune system by increasing the production of white blood cells, which are what helps your body fight infections. Spending time outside can easily increase your exposure to sunlight, and in turn, your vitamin D levels. Vitamin D is essential for bone health, immune function and the prevention of certain chronic diseases. 3. Better Sleep Sleep issues are a common concern among adults across the country. By taking some time to get outdoors every day, your sleep quality may actually improve at night. Being exposed to natural light during the day helps regulate your circadian rhythm, which is the body’s internal clock that controls sleep and wake cycles. 4. Stronger Social Connections Socializing in outdoor environments such as a walk with a friend, participating in an outdoor group workout class or attending one of Reno’s many community festivals. can strengthen your bonds with others. Outdoor activities create opportunities to spend quality time with family and friends, helping to improve overall emotional well-being. 5. Better Heart Health Spending time outdoors, especially while engaging in physical activities such as cycling or hiking, has a direct impact on heart health. Regular outdoor exercise can lower blood pressure, improve circulation and reduce the risk of heart disease. As an added heart-healthy bonus, the relaxing and stress-reducing effects of nature can also act as a key prevention piece against heart disease. In the Reno-Tahoe region, the outdoor possibilities are endless. Head over to VisitRenoTahoe.com for more ideas on how you can experience the expansive nature that lies within our region.
-
Managing Anxiety Around School Violence
Reviewed by Dr. Takesha Cooper, MD, MS, FAPA, Chair, Department of Psychiatry and Behavioral Sciences, Professor of Psychiatry at University of Nevada Reno School of Medicine, Chief of Behavioral Health at Renown Health Sometimes it feels like every time you turn on the news, there is a new report about violence in our schools. Instead of being able to focus on the typical youth growing pains of learning test-taking skills, dealing with physical body changes, navigating friendships and dating and figuring out grades and routines, our children instead must prepare to deal with active shooter incidents, bullying, gang presence and hate crimes. These are heavy weights for children to bear and simply preparing for the possibility of such events can affect their mental health. As adults, it’s important to recognize when our children are struggling with anxiety, and to equip them with healthy tools and resources to help manage it. How to recognize signs of anxiety in children Anxiety in children can present itself in several different ways, depending on the child. Oftentimes, younger children will suffer from actual physical symptoms. They may wake up with a stomachache or headache, or they may often feel tired or irritable. In pre-teens and teens, anxiety can take the form of behavioral changes. They may withdraw from social connections and activities or have trouble sleeping or eating. As a parent, it may be difficult to know what to do when you see your child struggling with anxiety over school violence. How can you help your child when you are trying to figure out the same answers for yourself? You should know, however, that one of the best things you can do for your child is to simply be there for them. Anxiety tries to convince us that we are alone in our feelings, creating a sense of isolation, guilt and shame. A hug, reassurance and open conversation can provide the comfort your child needs during times of anxiety. How to talk to children about school violence Some important things to remember when talking to your children about school violence are: 1. Present the facts: Many times, children receive information about school violence from unreputable sources. Social media, peers and even family members are not always the most accurate sources of data and facts. Take the time to confirm the main details to stop wild theories and accusations in their tracks. 2. Provide Reassurance: It’s okay to let your children know when you are sad or scared about school violence, but you should do so in an age-appropriate manner and follow up with honest parental reassurance. Keep your explanations of the violent incident short and tailored to the age of the child. Acknowledge their feelings and the current situation but be sure to remind them that there are rules, laws and people in place to protect them, should that protection ever be needed. You can empathize with their anxious thoughts and feelings but also remind them that you are there to take care of them and that it is not their responsibility as a child to worry about school violence. 3. Promote Open Communication: Don’t be afraid to have complicated conversations with your children. They are usually able to process more than adults give them credit for. Find opportunities to have one on one time with your child and guide the discussion towards their anxious thoughts and feelings. Actively listen and validate their feelings without escalating fear and remind them that you are a safe and trusted resource who will not dismiss or judge their feelings but promises to be there as a support system. 4. Prepare with the Necessary Tools: Help teach your children coping mechanisms such as deep breathing, yoga, mindfulness or journaling. They can also learn to process their thoughts through physical outlets such as exercise, sports or hobbies to help foster a sense of control and normalcy. 5. Practice Safety Routines: While it can be sad to acknowledge that bad things happen in the world, it can be empowering for children to learn that there are sometimes things they can do to help in a challenging situation. You can discuss safety measures at school and remind them of teachers, staff and first responders who are available to help. Additionally, some children find that role-playing emergency protocols can help them feel prepared and powerful. 6. Protect Their Media Intake: In today’s world, news and information are available 24/7, coming to us from numerous media platforms. For adults, this constant stream of content can feel overwhelming, and for children, it can be even more distressing—especially during times of crisis. Children may struggle to process the information they have been exposed to, and they may lack the ability to distinguish between factual reporting and sensationalism. This constant influx of bad news can take a toll on their mental health, and they may not even recognize that they’re feeling stressed. Limiting their media exposure is an important step in caring for their emotional well-being. Take Care of Yourself Each time you fly on an airplane, the flight attendants tell you to “put your oxygen mask on first before helping others.” This is important because, in order to think clearly and be helpful to others in need, you have to be able to breathe and function on your own. This adage also rings true when it comes to helping your children manage their anxiety. You must take care of yourself and manage your own fears and stress so that you can effectively provide guidance and support to your children. Remembering to eat properly, exercise, get enough sleep and find strategies to manage your own mental health are crucial to you being the best you can be, so that you can provide comfort to your child and advocate for their health and wellbeing. When to Seek Professional Help Remember that it’s okay to ask for help. If you find that you or your child are struggling with depression, anxious thoughts, persistent fears, loss of appetite, irritability, lack of desire to engage in life activities or with loved ones or other signs of distress, please reach out for professional help. Counseling, support groups and therapy with a licensed mental health professional are all effective ways to cope with these emotions and serve as a helpful reminder that no one has to face them alone. Click here for additional information about Renown Behavioral Health.
-
Department Spotlight: Hospice & Palliative Care
In the book of life, everyone eventually reaches the final chapter. End-of-life isn’t often something a patient or loved one wants to think about. The end of someone’s life isn’t a final option – it's a privilege. At Renown Health, we have a compassionate team prepared to approach this privilege with kindness and care. The Hospice & Palliative Care department at Renown is the best of the best. Their efforts go far beyond simply addressing physical pain; they also bring emotional and spiritual solace to patients and family members navigating the complexities of serious illness and end-of-life. This team provides crucial guidance and expert knowledge, comfort and care when it is most needed. Bringing Dignity to the Final Days Contrary to popular belief, hospice and palliative care is not a “last resort” option for families. In fact, it’s quite the opposite. These caring professionals work hard to ensure a patient’s final days are free of pain and full of peace, rather than focused on the end. This type of care isn’t a death sentence – it's a living gift. Each patient is involved in his or her own end-of-life process. They have a huge role in deciding on their own and with their family members how they want to live out their remaining days. “Every team member’s daily work focuses on how to facilitate a good death for each patient,” said Tanya Prosch, Hospice Supervisor. “Ultimately, it is up to each patient’s family to be involved in this process. Every day, there is a lot of communication among team members as we prioritize the needs of our patients. As patients decline and their symptoms change, we continuously assess what topics we will discuss. This creates a beautiful back-and-forth dynamic among the team, patients and families.” “Together, we come as a team to provide what they need, ensuring individualized care for each patient and family based on their safety and specific needs,” added Rachel Schneider, Transitional Care Specialist. “Our care plans are not cookie-cutter; they are tailored to fit each unique situation.” The hospice team provides comfort and support to those in the final stages of a terminal illness. Hospice is focused on one main goal, which is enhancing quality of life for patients and their families. “In general, hospice staff conduct home visits to see our hospice patients,” said Amy Nieminen, Manager of Home Health & Hospice. “We have an interdisciplinary team that includes nurses, aides, chaplains, social workers and volunteers. Together, we address both the physical and emotional, spiritual and social needs of our patients and their families at the end of life, ensuring they have a meaningful and peaceful experience. We do a lot of work with families and loved ones, providing follow-up calls and support for the patient’s caregivers after their passing. Our support extends for up to a year, with grief specialists available to help families through their loss. Additionally, we have rotating on-call nurses every night and weekend, so patients are never left without care.” While palliative care shares similar duties to hospice care, it differs slightly. Palliative care can be involved at any stage of a serious illness, even during treatments. “During in-home palliative care, we work with patients who may be physically ready for hospice but who are not yet psychologically, emotionally or spiritually prepared to make that transition,” said April Lennon, APRN for In-Home Palliative Care. “They may still be exploring treatment options and working with their specialists. We provide a lot of support, helping them understand the consequences and benefits of various treatments. Additionally, we focus on symptom management for patients experiencing significant pain or nausea, assisting them in managing these symptoms effectively.” On both sides of this department, the team has the opportunity to be especially involved in their patients’ lives and in the lives of their families. Giving loved ones more time with their relative facing end-of-life is a duty that these team members take seriously. “My job is to educate families about what’s coming next and what is happening now, as there is a lot that occurs during the death process,” said Katie Adams, Hospice Nurse Case Manager. “Families will never regret the time and effort spent during this process. We have only one chance to get this right. This is not just a random hospitalization that people will forget; it is a significant moment that everyone around the patient will remember.” “Being able to connect more deeply with patients’ and families’ stories and their narratives about life is essential, as it provides a broader understanding beyond just the medical picture of what is happening,” added Libby Krayk, APRN for Hospice. “We explore their expanded value and belief systems to assist with decision-making, helping them make choices together. When patients are no longer distracted by pain or nausea, they can focus on their long-term desires and goals and spend more time with their families." “Crisis intervention, social work, education, family conferences, and placement issues are all part of what we do, and it’s quite exciting,” added Donald Kamka, Social Work Care Coordinator. “You become fully invested in the lives of those you help, which is what makes this job so rewarding. This is a remarkable time in their journey, and it’s evident that everyone involved has a vested interest in it." Naturally, many questions, worries and fears arise during this time in a patient’s life. The Hospice & Palliative Care team members are expert communicators and know exactly how to relieve some of those anxieties, prompting a more peaceful end-of-life. According to this team, it’s all about transparency and compassion. “Our role involves helping patients navigate the healthcare system as they face death,” said April Lennon. “Home visits can range from one hour to three hours, depending on the needs of the patient and their family. We engage with entire families, including those who are out of town, coordinating care and working with many providers in the area. Our hope and goal for every patient is to ensure they understand what they are doing and why they are doing it, empowering them to make their own choices.” “We often find ourselves addressing the most difficult information, which can sometimes be seen as the ‘elephant in the room’ that people tend to avoid,” added Libby Krayk. “I ask patients for their permission regarding what they want to know and who they would like involved in the conversation. This approach can help alleviate some of the challenges and stress they may be experiencing. Being honest and discussing matters in a way that they can understand is essential. I take the time to sit down with my patients and connect with them on a human level, rather than just a medical level.” As a not-for-profit health system, volunteers are at the core of our mission delivery. They graciously dedicate hours out of their week to be a friendly source of help for patients. Renown’s Hospice Volunteers exude this level of kindness and more. Our employed team members attribute their volunteers as a major source of success for Renown’s hospice program. “I believe that being a volunteer provides a role that patients perceive as non-threatening,” said Linda Derry, Hospice Volunteer. “As volunteers, patients feel more comfortable talking to us and sharing things. This dynamic allows them the freedom to express not only how they are feeling but also their fears and any other concerns they may have. It is in these moments that we can truly connect with them, as we are volunteering out of a genuine desire to sit and visit with the patients. “When I see a patient, the focus depends on their specific needs,” added Luanne Geissler, Hospice Volunteer. “I often give family members some time to themselves to do whatever they need to do while I visit with the patient. Many of them are very talkative and eager to share their stories. For instance, one patient told me how to make a baked potato while out in the wilderness, which has become one of my favorite stories. Another patient shared her experiences about coming to America from Asia, discussing her church, her religion and her passion for baking. She would even bring bread to her doctor.” “I have one patient whose main desire is to play chess; he has been playing for over 80 years and is still able to play very well,” added Hervey Ibarra, Hospice Volunteer. “When I visit another patient at his home, we engage in conversations about a variety of topics. Additionally, some patients ask me questions about the military and law enforcement. Whatever they want to do and discuss, that is what I focus on during our time together.” Regardless of whether they are a provider, supporting team member or a volunteer, every person on the Hospice & Palliative Care team shares a primary focus: helping patients live their remaining days, no matter how long that may be, with dignity and comfort, surrounded by their loved ones.
Read More About Department Spotlight: Hospice & Palliative Care
-
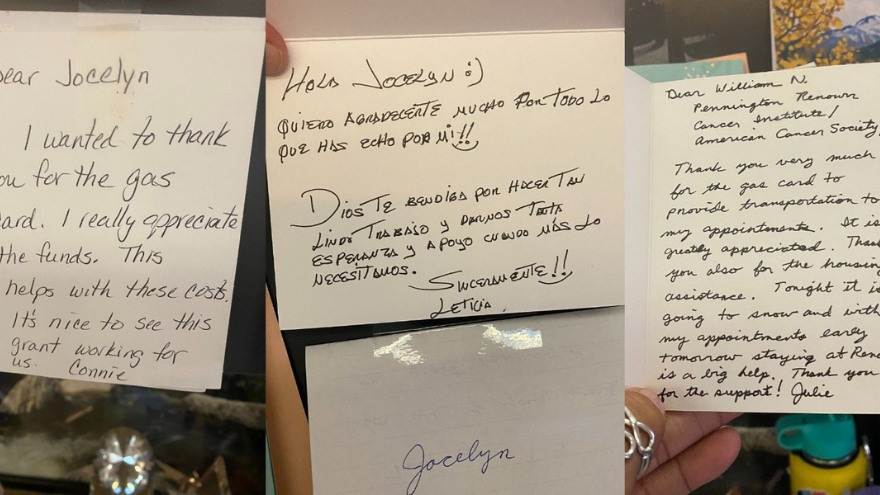
A Journey of Support: How Grants from the American Cancer Society Impact Patients at Renown
For many cancer patients, a significant hurdle is simply getting to treatment. Patients from Nevada and California often face considerable financial and logistical challenges when traveling for care. Limited resources for transportation and lodging can result in missed appointments, treatment interruptions and delays in follow-up care. To address this crucial need, Renown Health Foundation partners with the American Cancer Society (ACS) to ensure our patients can access the care they need by reducing financial barriers many patients face ACS awarded $70,000 to Renown Health Foundation last year. These funds, distributed as gas cards and lodging support to qualifying patients, have proven to be a lifeline in assisting those in need. Fueling Hope with Gas Cards Through our partnership with ACS, Renown supported 128 cancer patients over the past year. This assistance provided 2,260 round trips, ensuring that patients from Nevada and California could attend their critical treatments at the William N. Pennington Cancer Institute at Renown. These patients, aged 15 to 94, traveled up to 320 miles, sometimes from remote areas such as Tonopah, Elko and Susanville, for their cancer care “We're deeply committed to supporting our patients through every step of their journey, and our partnership with the American Cancer Society is instrumental in making that happen,” said Jocelyn Mata, Oncology Social Worker at the Pennington Cancer Institute. “Without them, we wouldn't be able to provide the crucial financial assistance that many of our patients need.” Jocelyn works with qualifying patients to provide gas cards and accommodations at The Inn at Renown, a hotel at Renown Regional Medical Center. She ensures they can focus on their treatment without worrying about the financial burden. Lodging Support for Peace of Mind Along with transportation aid, we can provide safe and comfortable lodging for qualifying patients. "We encourage patients to rest and, if they have a long journey home, to stay overnight," said Dr. Max Coppes, Director of the William N. Pennington Cancer Institute. "Providing lodging support ensures they have a safe and comfortable place to recover before making the trip back." This assistance is crucial for those who travel far from home, allowing them to focus on healing without the added stress of finding and affording accommodation.
-
Protect Your Child’s Health with Timely Vaccinations
Why are timely vaccinations important? Childhood vaccinations are scheduled and vaccines are administered when young bodies require immediate protection or need to build immunity for diseases and illnesses we may encounter throughout our lives. Delaying recommended vaccinations puts children at higher risk for diseases that can affect them more harshly, like pertussis (whooping cough), which is especially dangerous for babies. Vaccination Benefits Vaccinations save the lives of 1,000s of children (and adults) every year Vaccinations protect us from illnesses that can lead to cancer, hospital stays, life-long health issues & even death Vaccinations help protect those who receive the vaccines and, through herd immunity, also help protect the unvaccinated and seniors whose immunity may have waned. What’s the recommended vaccine schedule for children? In the U.S., we follow the CDC’s vaccine schedule for children and teens up to 18 years of age. The schedule also provides notes regarding missed or late vaccine doses and how to properly “catch-up.” If your child is missing one of the vaccinations listed below, is not quite on-schedule with the recommended timeline or you have any questions regarding vaccines or timings, please reach out to your child’s provider. Vaccine Schedule Birth to 4 Years: Birth – First vaccine for hepatitis B and may receive respiratory syncytial virus (RSV)* vaccine 2, 4 & 6 months of age – Vaccines/boosters for tetanus, diphtheria and pertussis (DTaP), polio (IPV), haemophilus influenza type B (HiB), pneumonia, hepatitis B and rotavirus 6 months to 4 years of age – COVID-19 vaccine, 1-2 doses* 1 year of age – First dose of measles, mumps, rubella with varicella for chicken pox (MMRV) vaccine and boosters for hepatitis A, HiB and pneumonia 15 months of age – 4th dose of DTaP 18 months of age – 2nd dose of hepatitis A 4 years of age – Final dose of MMRV, TDaP and IPV vaccines *Conditions apply. See your child’s provider. Vaccine Schedule 5 Years & Older: CDC and American Academy of Pediatrics (AAP) also recommend the following vaccine schedule for children as they grow: Prior to starting middle school – TDaP and meningitis vaccines/boosters 9-12 years of age – AAP suggests children (and those up to 26 years of age who have not been adequately vaccinated) receive the HPV vaccine to help protect against developing certain cancers as adults Children up to 18 years of age & adults – COVID-19 vaccines are recommended, especially for those with medical conditions such as asthma and diabetes For more vaccination information, please refer to the CDC recommended child and adolescent immunization schedule. Any tips on preparing my child for a vaccination? Many parents worry about side effects like pain and fever for their children after getting vaccinations. Studies have shown that giving Tylenol prior to vaccines can decrease their effectiveness. That’s why providers recommend parents and caregivers wait until after vaccines are administered before giving Tylenol or Ibuprofen, and then only if symptoms develop. Do vaccinations wear off? Many vaccinations provide life-long immunity while others may wear off over time. Vaccines are given to children when they are at most risk for contracting diseases as well as when they are at the highest risk of severe complications from a disease. So even if immunity fades over time, it is important receive vaccinations on time to protect children during these high-risk windows. Doctor's Advice: Ensure Your Child's Health with Timely Vaccinations A child receiving a vaccination can be a scary thing for some parents and misinformation about vaccines on social media and the internet can make things confusing. It is important for parents to discuss any questions they have about vaccines with their child’s health care provider. As medical providers caring for children, we all have the common goal of keeping children the healthiest they can be – and vaccines are an important part of that. To schedule an appointment with a Renown provider, please go here and click here to learn more about Brittany Lemons, MD.
Read More About Protect Your Child’s Health with Timely Vaccinations
-
How to Spot Depression in Men
Is a man in your life struggling with depression? Many men find it difficult to acknowledge when they need help. Recognize their unique warning signs of depression with insights from psychologist Dr. Herbert Coard. Over 6 million men are diagnosed annually, often displaying symptoms like anger and aggression instead of sadness. Learn how to support them and understand these often-misinterpreted indicators. Behavioral Signs of Depression in Men High levels of the hormone cortisol are released during stressful situations affecting the neurotransmitter, serotonin (a feel-good hormone), contributing to depression. You can identify depression or suicidal tendencies by paying close attention to the following behavioral changes: Anger, irritability, or aggression Avoiding family or social situations Losing interest in family responsibilities, passions and hobbies Lack of sex drive Becoming controlling/abusive in relationships Risk-taking behavior such as; unsafe sex, overspending or gambling Not being able to concentrate or remember details Excessive drinking or drug use Having frequent thoughts about death Talking about suicide Attempting suicide Factors That Lead to Depression in Men Life Events Work stress or long-term unemployment can be huge contributing factors relating to depression. This type of life event can be overwhelming, making it impossible for a man to cope. Changes in Relationships The loss of a relationship can be a significant contributing factor to the emergence of depressive symptoms and past experienced physical, sexual, or emotionally abusive relationships. With this in mind, counseling can often help individual to overcome this type of trauma. Grief and Loss Overwhelming sadness due to the loss of a loved one can trigger depression. Although normal, each person goes through their own grieving period. For example, normal responses to death are insomnia, poor appetite and loss of interest in activities. Pay attention if grief seems prolonged or out of the ordinary. Health Problems In particular, depression coexists with medical conditions. As men age, this can be passed off as normal aging, but it could be more serious. In addition, illnesses such as thyroid disorders, Addison’s disease and liver disease can cause depressive symptoms. Diabetes, cancer, heart disease, or Parkinson’s disease can affect any age, thus triggering or worsening depression. Some older men also feel like they may be suffering from dementia because of difficulties with memory this may be a symptom of depression. A trip to the doctor may be in order to help alleviate concern and worry. Depression in Men and Suicide Frequently the emotional pain occurring with depression can distort a man’s ability to see a solution beyond suicide. Individuals with depression become very rigid and constricted in the way they solve problems. The statistics below speak for themselves, helping us understand the need to reach out to those who need our support. Male suicide rates are on rising – men die by suicide 3.53 times more often than women, accounting for 70% of all suicides. Sadly, every day 129 men commit suicide. White males accounted for 69.67% of suicide deaths in 2017. In 2017, firearms accounted for 50.57% of all suicide deaths. Middle aged Men who are middle aged have the highest suicide rates. 40% of those identifying as transgender have attempted suicide in their lifetime. Males who are guy or transgendered are at an increased risk for suicide attempts, especially before age 25. Veterans often suffer from post-traumatic stress disorder (PTSD) and depression, and are more likely to act on a suicide plan. How You Can Help Now that you can identify some of the warning signs of depression, here’s how you can help: Talk about your concern and communicate that you’re there to help him. Let him know depression is a medical condition and will usually get better with treatment. Suggest professional help from a Primary Care Provider, Psychologist or Therapist. Help set up appointments and offer to accompany him – let him make the decision, but make it clear you’re there for him, no matter what he decides. If you feel he is in a dire or life-threatening situation, contact 911. Call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to talk to a trained counselor. Call the Veteran’s Crisis Line at 1-800-273-TALK (1-800-273-8255) and press “1”
-
When Should You Consider Hospice? 5 Important Signs
Deciding on hospice care for a loved one is a deeply personal and challenging decision, balancing their wishes and medical realities. Rebecca Edwards, DNP, from Renown Hospice Care, explains the signs indicating when it might be time for hospice and offers guidance on navigating this decision with compassion and clarity. Understanding Hospice Care Before exploring the decision-making process, it’s crucial to have a clear understanding of what hospice means. Hospice care represents a shift in how we approach living with a terminal condition, emphasizing comfort, dignity, and quality of life above all else. When there is no longer a pathway to a cure, side effects of treatment outweigh the benefits, or someone is simply tired of frequent hospital visits, then it may be time for hospice. Hospice care is mainly done in the home, where most people wish to be. It's a compassionate, team approach to care that focuses on meeting the physical, emotional, and spiritual needs, supporting their families, and honoring individual preferences. 5 Critical Signs to Be Aware Of Decline in Overall Health: When a loved one's health continues to decline despite ongoing medical interventions, this may be a sign that these treatments are no longer effective. Increasing Pain and Symptoms: When managing symptoms such as pain, nausea, fatigue or shortness of breath becomes increasingly challenging, hospice can offer specialized support and expertise in symptom management. Frequent Hospitalizations: Repeated hospitalizations or emergency room visits can signify that the disease has progressed to a point where managing symptoms and providing comfort at home or in a hospice setting is a more appropriate approach. Difficulty with Daily Activities: If your loved one is experiencing difficult with activity of daily living such as dressing, bathing, or mobility, it may be a sign that they require additional support and assistance. Prognosis of Six to 12 Months: Hospice Care is typically recommended for patients with a prognosis of about one year or less if the disease follows its normal course. However, it’s important to remember that every individual is unique and prognosis can vary.
Read More About When Should You Consider Hospice? 5 Important Signs
-
Why Childhood Immunizations Are So Important
Immunizations save thousands of lives each year by preventing serious illnesses, hospitalizations, and deaths. They also protect those who can't be vaccinated, like young children and the elderly, through herd immunity. Renown Pediatrician Dr. Kristin Wilson highlights the crucial role of vaccines. Immunizations Your Child Needs (and when) Birth to 6 Months Hepatitis B: Shortly after birth, first vaccine dose Diphtheria, Tetanus, and Pertussis (DTaP), Polio, Haemophilus Influenza (HiB), Pneumonia, Hepatitis B and Rotavirus: Ages 2, 4 and 6 months, boosters and vaccines One Year to 18 Months MMR and Varicella (chickenpox) vaccine: Age 1, first vaccine dose Hepatitis A, HiB and Pneumonia: Age 1, booster DTaP: 15 months, fourth vaccine dose Hepatitis, second dose: 18 months Flu Vaccine: 6 months and older, annually* *In the year after receiving their first dose, an infant will need a booster one month later. Four Years Old MMRV, DTaP and Polio, final dose: Four years of age Pre-Teen and Beyond Tdap and Meningitis: Before starting middle school, children receive these vaccines. They are also old enough to start the HPV vaccine, an essential vaccine for all young adults to protect against cancer, genital warts and cervical dysplasia.
Read More About Why Childhood Immunizations Are So Important
-
Life after Lymphedema Diagnosis: What to Expect
Managing lymphedema effectively is essential for enhancing the quality of life for individuals affected by this condition. Katherine Bunker, a Physical Therapist and Certified Lymphedema Therapist (PT, DPT, CLT) at Renown, has expertise in this area and her insights offer valuable strategies for managing lymphedema. Lymphedema is a chronic condition characterized by swelling in one or more limbs due to a blockage in the lymphatic system. This condition can result from cancer treatments, surgery, infection, or can sometimes be congenital. While it can be challenging to live with lymphedema, understanding the condition and adopting specific lifestyle changes and strategies can significantly improve the quality of life. Understanding Lymphedema Educating yourself about lymphedema is crucial. Understanding the causes, symptoms, and potential complications can provide you with the tools to manage the condition proactively. Lymphedema can lead to discomfort, decreased mobility, and in severe cases, infections such as cellulitis. Therefore, recognizing the early signs and knowing when to seek medical advice is essential. Medical Management Consulting with healthcare professionals who specialize in lymphedema is critical. A physiotherapist or occupational therapist trained in lymphedema management can tailor a treatment plan for you that can include the following: Compression Therapy - Wearing prescribed compression garments can help move the lymph fluid and reduce swelling. It’s essential to get fitted by a professional and understand how to use these garments correctly. Manual Lymphatic Drainage (MLD) a gentle massage technique that encourages the movement of lymph fluid out of the affected limb. It’s typically performed by a trained therapist but ask about self-massage techniques you can do at home.
Read More About Life after Lymphedema Diagnosis: What to Expect
-
Department Spotlight: Renown Health Foundation
Kick off 2024 with us as we celebrate the team behind our very own Renown Health Foundation! When you visit Renown Health, you take a look around and can’t help but notice the robust programs in place. You look left and see our thriving Children’s Miracle Network Hospital at Renown, making a lasting impact on pediatric healthcare in our region. You look right and see the advanced William N. Pennington Cancer Institute, providing leading-edge treatments right here in our community. You look around you and notice an influx of smiling nurses from the Orvis School of Nursing at the University of Nevada, Reno (UNR) who receive tuition assistance, thanks to generous donations to the Gerald “Jerry” Smith Academic Practice Partnership. Then, you think to yourself: “These programs must need a lot of money and support. So, how on earth is this all possible?” What you may not know is that these programs are funded by the generosity of our community, all made possible by the work of Renown Health Foundation. As the largest not-for-profit health system in northern Nevada, our mission to make a genuine difference in the health and well-being of everyone we serve flourishes because of the donations, sponsorships, endowments and more that our Foundation brings in from philanthropists all over the region. Making It Happen The reach of Renown Health Foundation has proven to be virtually limitless, with a clear focus on supporting and raising funds for programs and initiatives that enhance the lives of our patients and their families, all for the betterment of our community for years to come. Under their growing umbrella, the dedicated team at the Foundation makes miracles happen through administering a wide range of philanthropic programs, including: Children’s Miracle Network Hospitals (CMNH), a nonprofit organization that supports the health of 10 million children in the U.S. and Canada every year. Renown Children’s Hospital is proudly recognized as a member of CMNH. Gerald "Jerry" Smith Academic Practice Partnership, a partnership between Renown Health and the UNR Orvis School of Nursing to provide 24 nursing students a year with full-ride tuition assistance and a guaranteed career in nursing at Renown. Fianna’s Healing Garden, a healing garden bringing serenity to all at Renown Regional Medical Center, built from the vision of Fianna Dickson Combs. Miracles at Montreux Golf Tournament, an annual golf tournament that takes place at Montreux Golf & Country Club and consistently raises hundreds of thousands of dollars for Renown Children’s Hospital. A full slate of individual giving programs, including Legacy Giving, Employee Giving and Leadership Giving. But it doesn’t stop there – the Foundation is helping our health system build more ways to care for our community by securing major gifts to fund advanced healthcare facilities and innovative healthcare solutions: William N. Pennington Cancer Institute, the premier oncology institute in the region providing a large array of personalized cancer care services, including Medical Oncology, Infusion Services, Clinical Research and more. Renown Institute for Robotic Surgery, offering the latest advancements in surgical technology with robotic-assisted surgeries, which ensure precision, faster recovery and improved outcomes. Sophie’s Place, a state-of-the-art music therapy room currently in construction at Renown Children’s Hospital. This new space will be specially designed for children and their loved ones to enjoy the healing power of music and engage in the arts. Conrad Breast Center, the latest addition to the planned Specialty Care Center at Renown South Meadows Medical Center which will include breast imaging, infusion and surgery services along with a wellness center. Jeanne and Raymond Conrad donated a $5 million lead gift to support this important project and the Foundation team is currently working to raise an additional $6 million in 2024. It may go without saying that a day-in-the-life of these spirited team members is never a dull one. Every day brings on a new challenge to face and a goal to meet. “A day at the Foundation is a day full of emails, calls and visits with friends of Renown,” said Abbey Stephenson, Planned Giving Officer. “Our main goal is to raise funds to support the mission of Renown, and most of our outreach efforts are to encourage philanthropy and donations. We have a very collaborative team, so we can often be found in each other’s offices strategizing about fundraising initiatives, communications and next steps with specific supporters.” “For me, a typical day involves making sure I have a donor scheduled for coffee or lunch, working on proposals that may need research and preparing presentations,” added Jerry Cail, Major Gifts Officer. “Staying connected, I send thank you notes for any donations-usually once a week and make at least three ‘Grateful Patient’ calls to set appointments. I always make sure I am ready to contribute to any meetings I have for the Foundation." While the scope of the Foundation’s charitable efforts goes beyond hospital walls, they also thrive right here in our own health system. Through our Grants Program, Renown’s departments and programs can leverage the connections and skills Renown Health Foundation has in order to secure funding from a multitude of grant sources. "Grant funds from foundations, and local, state and federal governments benefit the patients and communities we serve to further our mission, vision and values,” said Pam Citrynell, Development Officer. “Past grants have supported the purchase of state-of-the-art equipment, facility development, pandemic recovery, research and clinical trials, physician and researcher recruitment, community health programs and educational training for our healthcare professionals.” Every Foundation team member lives their passion every day while at work, frequently expressing gratitude for the immense impact they have the opportunity to make. “I love coming to work because I get a very real opportunity to make a genuine difference and meet some fantastic people who believe in and support our mission,” said Leah Nelson, Director of Community Giving. “I have had the honor of meeting donors and the families they support. I couldn't be prouder of what our team has accomplished over the years and am excited for what is to come.” The impact of the Foundation team’s tireless efforts extends far into the future, securing Renown’s lasting legacy in contributing to the continued health and well-being of our community. “Philanthropy is not only a financial science but a very specific methodology where connecting resources are paramount; it requires careful intelligent management coupled with lots of hard work, patience, and vision,” said Yvonne Murphy, Development Officer. “The work that the foundation does every day makes resources available to enhance the healthcare experience for all those who seek care at Renown. Our work impacts not only this present moment but in fact is a legacy that will bless this community beyond our lifetime.”
Read More About Department Spotlight: Renown Health Foundation
-
Department Spotlight: Children’s Infusion Services
Help us celebrate the holiday season by sharing joy with our Children’s Infusion Services team! Thinking about blood can make any of us squeamish, and seeing it can be even more intimidating to the children in our lives. Being treated for a condition that requires blood transfusions or chemotherapy infusions is no easy feat, especially during the holiday season. This time of year, we are proud that we can offer our pediatric patients the power of proximity and excellence by having access to high level care close to home. The Children’s Infusion Services (CIS) department at Renown Children’s Hospital is committed to bringing the gift of quality care to our community’s youngest patients. Whether they are caring for a child with a blood disorder or giving expert infusion care for a child battling cancer, no team does what they do better than these expert nurses, medical assistants, intake coordinators and physicians. ‘Tis the Season to Bring Hope As the only pediatric oncology and hematology program in the region, the CIS department has a lot of responsibility on their shoulders. From inpatient chemotherapy to outpatient infusion services, this team treats a long list of pediatric blood conditions including: Pediatric cancers Anemias Immune-mediated blood disorders Sickle-cell disease Bone marrow failure syndromes Bleeding disorders “Our team provides a large variety of services from labs draws, sedations for procedures, infusions for diagnoses such as Crohn's disease, blood transfusions, as well as chemotherapy,” said Jen Torres, RN. “Our team works extremely well together. We try to go above and beyond for our patients every day. It may be something as simple as a hug to comfort a parent or a special birthday gift for a patient.” “My job allows me to work with several departments and providers when coordinating care for our littlest of patients,” added Jane Strawn, Intake Coordinator. “I assure proper authorizations are in place for the care that is needed, I communicate with our families when scheduling appointments, I organize End of Treatment Celebrations, as well as birthday shout outs and work closely with our Child Life team to help make the challenging appointment little easier.” To best serve their patients, the team thrives on being expert multitaskers. Central line care, chemotherapy administration, blood transfusions, medication management, preventative injections, lab draws, lumbar punctures, biopsies, imaging – you name it, they do it. And they do it all with the utmost focus on safety and support. “Our days have a lot of variation, as we perform a number of different services,” said Meagan Bertotti, RN. “We provide infusions for patients with chronic or acute medical conditions and chemotherapy/biotherapy treatment to patients undergoing cancer treatments. Overall, though, we work as a team to make these difficult procedures and treatments as easy as possible for the patients and families by providing engagement and support.” “While we handle a lot of chemotherapy treatments for pediatric patients, we also do other infusions and transfusions as well such as blood and platelet transfusions, enzyme replacement therapies, different types of injections such as Rabies vaccine or Synagis for high-risk babies who need that extra protection during the RSV season, and lab draws,” said Chelsea Angues, RN. “We care for patients that get their therapies from outside hospitals, but the patient lives within the Reno area. We receive orders from those outside hospitals to care for those patients, so they can still be with their families and not have to travel.” As members of the Children’s Oncology Group, a highly-regarded clinical trials group where over 90% of pediatric cancer patients across the U.S. receive treatment, teams like CIS in Renown Children’s Hospital deliver the highest standard of care. This partnership is a true testament to the devoted collaboration and relationship-building this team commits to on behalf of their patients every day. "One of the biggest accomplishments of our team is the fact that we became a member of the Children’s Oncology Group, and the Children's Infusion Center and Pediatric Oncology became one unit,” said Shelby Nolte. "Instead of being a clinic on one side and an infusion center on the other, we really came together to make it a whole unit that collaborates on almost everything.” “We've put much time into trying to understand other departments, their flow, their rationales and their processes so we can come to a solution that benefits our patients the greatest,” added Tiffany Macie, RN. “We've taken the last few years to really build our relationships with our pharmacy staff, our lab staff and our central supply resources. Our relationship building extends beyond the walls of the Renown building as well and out to the community providers too. In the past few years, we've been able to build relationships with the providers in the community where they trust they can send us their patients for treatment and lab draws. Finally, we've spent much time working on the relationships as a team. It's emotional work we do on our unit, and these families become our family. It's important to us that we take the time to be together outside of our shifts to enjoy one another and laugh!” In the compassionate realm of pediatric healthcare, CIS knows that the complexities of a cancer or blood disorder diagnosis can take an emotional toll on their patients and families. The team firmly believes that emotional support can be as important as the physical and medical support throughout each patient’s unique care journey, striving to be a comforting presence during daunting times. “The most important part of my day is collaborating with the Children's Infusion team to make life manageable for the families that are going through this experience,” added Shelby Nolte, Senior Medical Assistant. “We work as a team to make life easier for the blow of a cancer diagnosis. We are there for our families in every way. If they need a shoulder to cry on, an ear to listen or just someone to play cards with or tell a funny story too, we are there.” “One of the things our team does extremely well to help our patients and their families with new diagnoses is to simply meet them where they are,” said Tiffany Macie. “That looks different for every family and every patient. We work in an environment where can build relationships with our patients and their families. This allows us the unique opportunity to really get to know them. We learn their fears, their joys, their worries, what their family lives are like, and we learn how to best meet them where they are.” Transcending the conventional boundaries of care, the CIS department closely supports each patient, offering them solace tailored to the unique fabric of each family's life.
Read More About Department Spotlight: Children’s Infusion Services