Search
Results for 'doctors'
Clear-
MyChart Proxy Access
What is Proxy Access? Proxy access allows parents, legal guardians and caregivers to log into their personal MyChart account and connect to the health information of a patient they represent. As a proxy, you can view upcoming appointments, request appointments, view lab results, email a doctor on the patient’s behalf, view medications, request prescription refills and view health reminders. How Do I Establish Proxy Access? Login to your MyChart account with your username and password Go to the Profile menu at the top of the screen, then select Personalize From this screen you can see whose records you currently have access to Click Request Access to a minor’s chart Complete all of the fields When finished click Submit Request What if I Don’t Have a Renown MyChart Account? If you don’t have a Renown MyChart account, call 775-982-2781 and someone from the Renown Health MyChart team can help you set up proxy access. Keep in mind, the ability to request proxy access is only available on the MyChart website and not via the mobile app. However, the website can be accessed with your smartphone or tablet by using the web browser and going to mychart.renown.org.
-
Why I Give: Margo and Jim’s Story
Lifetimes of Service in Medicine Margo and Jim Veazey are no strangers to hospitals and medicine. They are impressive duo with notable professional achievements and seem to always have service to their communities and country as their true north. Margo was a nurse and nurse administrator for her entire career, which spanned just under 50 years, including 25 years in nursing leadership at the Connecticut VA Healthcare System. Her predecessors at the VA had only stayed a year or two prior to her, but Margo found a place where she could make a positive impact and stayed for a quarter-century. During her time at the VA, she helped secure a much sought after $40 million grant to establish a VA Nursing Academy including funding for five new faculty members. The groundbreaking program to educate and train more nurses shares some strong similarities with Renown’s recently established Gerald “Jerry” Smith Academic Practice Partnership. Jim has had his own esteemed medical career of over four decades as an infectious disease doctor, serving in academic, clinical and research roles on the east coast. He retired from the U.S. Army as a Colonel after 29 years of combined Federal Service in 2012. Among his self-stated greatest achievements was working on the eradication of Smallpox in India (coincidentally, Renown was founded in 1862 during a Smallpox outbreak). A Near Death Experience Rarely had the Veazeys been on the receiving end of trauma care, but that all changed in 2017 after their move to Reno, when Margo was admitted to the Renown Regional Emergency Room with a volvulus, an obstruction caused by twisting of the intestine and a very serious medical emergency. The symptoms that led her to the ER were severe and extremely uncomfortable: fever, severe abdominal pain, overly active bowel sounds, and vomiting blood. Margo recalls: “the last thing I remember was hearing someone say my pulse was down to 20. I thought I was dying and then I blacked out. I woke up two days later in the ICU [Intensive Care Unit] as they told me to breathe out when they were removing my ventilator tube.” Jim, on the other hand, remembers it all, including the long hours waiting for Margo to wake up. Margo’s near-death experience left quite an impression on both of them and, while traumatic, it also created deep feelings of gratitude for the care Margo received from her doctors and nurses at Renown during that time. Reno Becomes Home Margo and Jim spent most of their lives on the east coast. They met at Dartmouth when Jim was a wide-eyed intern in the ICU, and Margo was working in the ICU as a nurse. They were married a year later and recently celebrated their 52nd wedding anniversary! You don’t have to spend much time with them to see their adoration for each other, even after all these years. In the midst of their busy careers, the Veazey’s raised a son and daughter, who now each have children of their own. Being closer to those grandchildren became a priority after Jim and Margo retired, which prompted their move to Reno in 2016. Having access to good healthcare was on their radar when deciding where to move, and they were not sure what they would find when they arrived in Reno. Fortunately, a neighbor they met early on introduced them to Renown and the Renown South Meadows Medical Center emergency room as an option for emergency care. It was not long after that, when Margo made a visit to the Renown South Meadows ER for diverticulitis. They’ve been coming to Renown ever since for her care. Expressing Their Gratitude Margo’s visit to the South Meadows ER in 2016 and her near-death experience in 2017 were among the first in a series of unfortunate and mostly unrelated health incidents she has faced since moving to Reno. Over the past eight years she has come to Renown for eleven major health issues including six surgeries. Her medical conditions have ranged from breast cancer to the need for a knee replacement to atrial fibrillation, and Renown has been a one-stop shop to meet her these urgent health care needs. Based on the trust she has in Renown providers, Margo counts on Renown for her preventative care too. Thanks to his long federal service, Jim receives his care at the VA. The consistency in the high-quality, compassionate care she receives—Margo and Jim will both tell you repeatedly how much they love Renown physicians and how great the nurses are—is why they keep coming back. When asked if they recall any specific doctors or nurses, Margo responded, “we’ve been to the emergency room so many times and I’ve had so many procedures that it would take a long time to list all their names, and I received wonderful care from all of them. My brother, who was a Rhode Scholar, emergency room doctor in Florida, and a lawyer was incredibly complimentary of the care I received when he was here during one of my ER visits.” The exceptional care is also what prompted them to include a gift to Renown Health Foundation in their estate plan. Although the Veazeys have always been charitable and support many organizations near and dear to them with annual gifts (including Renown Children’s Hospital), their legacy gift to Renown was the first time they included a charity in their estate plan.
-
How to Safely Give Children Over-the-Counter Medications
How can you ensure you’re giving your children safe doses of over-the-counter medications? The safest bet: Confirming dosages and recommendations with your doctor. With that in mind, here are a few answers to basic questions about OTC medications and children. It’s cold and flu season in Northern Nevada. This means you’ll find parents in the aisles of practically every drug store, wondering what will and will not work for their sick children. Over-the-counter (OTC) medications — and their dosages, side effects, interactions and more — can inspire abundant anxiety for parents. At the outset, the U.S. Food and Drug Administration offers the following warning about use of medicines for cough and colds in children: The FDA doesn’t recommend over-the-counter medicines for cough and cold symptoms in children younger than 2 years old. Prescription cough medicines containing codeine or hydrocodone are not indicated for use in children younger than 18 years old. Codeine and hydrocodone are opioids that are available in combination with other medicines, such as antihistamines and decongestants, in prescription medicines to treat cough and symptoms associated with allergies or the common cold for adults. Caregivers should also read labels on OTC cough and cold products, because some might contain codeine. So how can you feel comfortable administering any OTC medication to your children? The short answer is: Check with a doctor first. And with that in mind, here are a few common questions and answers from Kristin L. Wilson, MD, of Renown Pediatrics about children and OTC medications. Please talk about the importance of correct dosage of pediatric medications. Pediatric dosing is weight-based and unique to each medicine (and sometimes even the circumstance you are treating.) Therefore, there are no standardizations of “safe” amounts that apply to all medications. What are signs of an overdose of pediatric medications? Signs of intoxication/overdose are also unique to each medication and supplement. And to make it more confusing, mixing current prescriptions with various supplements or over-the-counter medications can cause significant adverse effects as well. Is there an age at which children take adult over-the-counter medications? Infants through adolescents can take medications that are also prescribed to adults, but only under a healthcare provider’s careful guidance. Dosing is determined by various factors dependent on child’s age and also medical history, as above. What is the takeaway about administering medications to children? When in doubt, ask a healthcare professional whether a medication or supplement is safe for your child based on his/her age and medical history as well as recommended dosing based on recent weights and other vital signs.
Read More About How to Safely Give Children Over-the-Counter Medications
-
5 Ways to Prevent Diabetes
November is National Diabetes Month, and with cases of the disease at an all-time high in the U.S., individuals must do everything they can to stay healthy. Learn more about diabetes prevention and also how to stop prediabetes in its tracks with these five helpful tips. Diabetes is a disease that is increasingly making its way into the public consciousness, and not in a good way. In fact, according to USA Today, diabetes has a greater health impact on Americans than heart disease, substance use disorder or COPD, with 30.3 million Americans diagnosed with the illness — and many more who are at risk for developing it. And those with prediabetes are at risk for developing type 2 diabetes in 10 years or less, according to the Mayo Clinic. The American Medical Association notes that 4 million U.S. adults have prediabetes. Check out the American Diabetes Association’s prediabetes risk test. The good news: There are ways to manage — and even reverse — prediabetes. Renown’s Certified Diabetes Educator Stephen Compston, RD, LD, CDE, shares five steps for managing blood sugar and also avoiding an eventual diagnosis. How to Prevent Diabetes Eat healthy foods. Plan meals that limit (not eliminate) foods that contain carbohydrates, which raise your blood sugar. Carbohydrates include starches, fruits, milk, yogurt, starchy vegetables (corn, peas, potatoes) and sweets. “Substitute more non-starchy vegetables into your meals to stay satisfied for fewer carbohydrates and calories,” Compston says. Exercise. Blood sugar is the body’s basic energy source. When you exercise, you are lowering your blood sugar. “People with prediabetes usually want to stay off of medication, so they must add something to their normal regimen that lowers blood sugar,” Compston says. “In this case, exercise is medicine.” Lose weight. A small decrease in your weight can drastically decrease your risk of developing diabetes in the future. The Diabetes Prevention Program study showed that a 7 percent decrease in body weight (14 pounds for a 200 pound person) can reduce a person’s risk of developing the disease by 58 percent. Get more rest. Studies link sleep issues to an increased risk of insulin resistance. It can also make it harder to lose weight. Thus, people that don’t get adequate sleep are at an increased risk for developing type 2 diabetes. See your doctor regularly. Schedule an appointment with your primary care provider at least once a year so you can track your health together. “A regular check-up and lab work can help identify what your blood sugars are doing so you and your doctor can develop a good plan for delaying the onset of diabetes,” Compston says.
-
Jakob’s Journey at Renown Children’s Hospital
In August 2016, six-year-old Jakob was admitted to Renown Children's Hospital with what seemed like a common ear infection. Jakob's condition quickly progressed, and he started experiencing neurological symptoms such as difficulty speaking and a full-body shutdown. Doctors, neurologists and specialists from Renown worked with doctors from Stanford, where he was ultimately diagnosed with Bickerstaff brainstem encephalitis (BBE). BBE is a rare, autoimmune response that attacks the nerves in the body due to an acute illness such as a cold, flu or, in Jakob's case, an ear infection. Jakob could not breathe or eat and experienced paralysis on the side of his face, throat, stomach, bowels, lungs and legs. In addition, he started to rapidly lose weight as well as body function. Jakob lost half his body weight which resulted in the need for a Gastrostomy tube. This device is placed surgically and gives direct access to the stomach to give the child the nutrition needed. He also needed occupational therapy, and after three and a half months of ICU respiratory therapy, surgeries and treatments, he was released home to regain his strength. Forever Grateful Anica, Jakob's mom, said, "If it were not for the quick response and unconditional support and compassion from the team at Renown, Jakob would not be here today." Jakob's family is forever grateful to the staff, community and expertise at Renown for their unwavering commitment to their son and family during their most trying time in life. "When I met Jakob on the first day of his illness, so much was unknown. My team and I were worried, as his symptoms were very unusual. His rapid deterioration, after being a perfectly healthy child, was clearly terrifying for his parents. Handing over a child's care to a team of strangers is one of the scariest things that can happen to parents,” said Dr. Kris Deeter, Physician in Chief at Renown Children’s Hospital. “However, Anica and Jeremiah were also very clear that they did not want Jakob transferred somewhere else. So, we used all our resources to care for him, arrive at a diagnosis, and start aggressive therapies. They listened to every word we said, educated themselves, and became partners in Jakob's care. We all became part of Team Jakob, and soon, he proved to us just how strong he was." Today, Jakob is 13 years old and thriving in every aspect of his life. He is currently on the honor roll in school and finds joy in his newfound passion for the violin. He loves spending his free time learning about mixing music, making new friends and traveling to different parts of the country. This summer, he will travel to Europe to explore his passion for culture. The family says, "We owe it all to the family and staff at Renown."
Read More About Jakob’s Journey at Renown Children’s Hospital
-
Protect Yourself and Others with the Flu Shot
Flu shots don’t just protect those who get vaccinated; they protect everyone, including your family and the community. As we continue navigating the COVID-19 (coronavirus) pandemic, Renown Health infection prevention expert Whitney Robinson explains how getting your flu shot is vital for staying healthy. 5 Ways to Schedule Your Flu Shot Call Us! 775-982-5000 Urgent Care Appointments Renown Pharmacy Vaccinations Make an Appointment via MyChart Need a Doctor? Find One Now Reasons to get the flu shot Chills, body aches, fever, congestion; getting the flu isn’t fun. But in addition to protecting yourself with a flu shot, you’re helping reduce flu cases and hospitalizations, Whitney said. Flu shots are currently available at pharmacies throughout the Reno area. Whitney says the ideal time to get your flu shot is September through October, but remain relevant throughout the winter months as it only takes two weeks for the antibodies to develop in your body. This timing allows the vaccine to provide the strongest protection during the length of flu season. Who needs a flu shot? Almost everyone. The Centers for Disease Control and Prevention recommends the yearly flu shot for everyone six months of age and older. Equally, they consider it the first and most crucial step in protecting against the flu virus.
Read More About Protect Yourself and Others with the Flu Shot
-
A Cancer Diagnosis and a Move to Reno
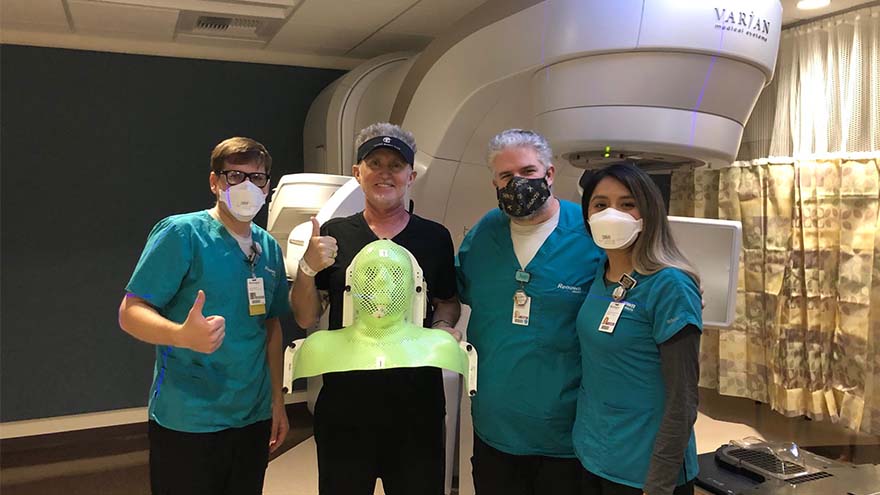
Michael Millman was all set to move to Reno from the Bay Area when he noticed a pimple-like growth on his forehead, and he decided to get biopsied "just in case." It was July 2020, less than six months into the COVID-19 pandemic, when Michael got the call that the biopsy came back cancerous. He was in shock. Still living in the Bay Area at the time, he immediately scheduled to have the basal cell carcinoma removed in August. After the removal, he thought he was in the clear, but a few months later, Michael noticed that his lymph nodes felt weird, and he even cut himself shaving because of some persistent swelling in the area. Given his recent history of skin cancer, Michael immediately scheduled an appointment with a specialist in the Bay Area. "I met with an ear, nose and throat doctor who suggested a fine needle biopsy of my lymph nodes, tongue and an MRI, both with and without contrast," Michael said. "I remember feeling dreadful and that I couldn't believe this was happening yet again." A Hard Decision Michael's squamous cell carcinoma, determined by the pathology report to be significantly influenced by the HPV virus, had metastasized to his lymph nodes on both sides of his neck, and his doctor said it could be stage four cancer. He remembers feeling like he was in quicksand, unsure if he should follow through with his move to Reno, or stay in the Bay Area for treatment. By now, it was early December 2020, and hospitals in the Bay Area and across the world were at limited capacity due to COVID-19. But, in what Michael describes as a positive twist of fate, the San Francisco ear, nose and throat provider he had seen about his biopsy results mentioned that he knew many providers in the oncology department at Renown, including Abhinand Peddada, MD. The San Francisco provider called Dr. Peddada's office with a referral, and Michael even remembers that Renown called him to hear more about his diagnosis before he even got the chance to call them "To be honest, I was feeling shut out in the Bay Area, and Dr. Peddada said he could help me expedite the treatment process," Michael said. "I finally felt a sense of relief." And so began Michael's 7-week chemoradiation cancer treatment program at Renown.
-
Hiking Through Life After TAVR
Renown Health patient, Alden Nash, hiking Death Valley National Park just three months after a Transcatheter Aortic Valve Replacement. Alden Nash isn’t your average 80-year-old. For much of his life, he could be found outdoors enjoying nature and hiking some of the west coast’s highest elevations. A husband and father of two, Alden turned his passion into a career as a Yellowstone park ranger in 1965. Alden believes his passion for the outdoors is responsible for his many years of health – until the unavoidable happened. The Hardest Climb The number one doctor recommendation for a healthy heart – lead a healthy, active lifestyle. Any cardiologist would be thrilled to have Alden as a patient due to his robust physical activity regimen. “Don’t have a TV set or a lounge chair in your house and you’re all set,” said Alden when asked how he has remained so fit throughout his senior years. Unfortunately, many other factors come into play when it comes to heart health, one of which is the reason we are telling Alden’s story today. Familial history - it’s a hot topic in the world of medicine. Understanding your genetic risk factors can help care providers develop updated care plans based on your results. Alden’s family has a long history of high cholesterol, which he avoided for much of his life by staying active. This combined with his age resulted in his first heart attack in December 2021. Doctors later determined that Alden was suffering from a type of heart valve disease known as aortic valve stenosis. Aortic stenosis is the narrowing of your aortic valve opening that impedes normal blood flow. Over time, the leaflets of your aortic valve become stiff, reducing their ability to fully open and close. When the leaflets don’t fully open, your heart must work harder to push blood through the aortic valve of your body. Eventually, your heart gets weaker, increasing the risk of heart failure. People who are most at risk for aortic stenosis include those who have had certain heart conditions present at birth, have chronic kidney disease or have heart disease risk factors such as high cholesterol and high blood pressure. However, generally, aortic stenosis is a degenerative process of aging with no modifiable risk factors. The incidence of aortic stenosis increases rapidly with age and is very common above the age of 80 – with 1/10 having the condition and 1/50 with a problem severe enough to warrant surgery. When symptoms are present, the disease can be rapidly disabling or even deadly, often progressing over several months unless treated.
-
Prestigious Honor Shines National Spotlight on Health Care in Nevada
Renown Health CEO, Dr. Tony Slonim Elected to Highest Office with American Hospital Association. Renown Health President and CEO, Anthony Slonim, M.D., DrPH, FACHE, has been elected to serve as a member of the American Hospital Association (AHA) Board of Trustees for a three-year term beginning Jan. 1, 2022. The Board of Trustees is the highest policymaking body of the AHA and has ultimate authority for the governance and management of the organization. The American Hospital Association (AHA) is the national organization that represents over 40,000 individual members and serves over 5,000 hospitals, health care networks, and their patients and communities. As a representative and advocate for those serving in the health care field, Dr. Slonim's role as a Trustee will be to ensure that members' perspectives and needs are heard and addressed in national health policy development, legislative and regulatory debates, and judicial matters. Dr. Slonim joins an elite list of CEOs from the nation’s most respected health care organizations in AHA Board service, including Yale New Haven Health (CT), Dartmouth Hitchcock Health (NH), Providence Health (WA), Henry Ford Health (MI), UMass Memorial Health (MA), Vanderbilt University Medical Center (TN), and Advocate Aurora Health (WI). The American Hospital Association was founded in 1898, the same year Marie Curie began studying uranium as a treatment for cancer. Dr. Slonim is among the first health care leaders from Nevada elected to serve on the AHA Board of Trustees. In an announcement to the national media, the AHA wrote, “Anthony Slonim, MD, DrPH, leads Renown's charitable mission of making a genuine difference in the community's health and well-being for one of the nation's most innovative and progressive health systems.” Steve Sisolak, Governor of the State of Nevada, in support of Dr. Slonim’s nomination wrote, “Both Dr. Slonim and I share a common interest for improving the health of over 3 million residents of our state. I urge you to appoint him to this position, as his national leadership would benefit the American Hospital Association, our state and our nation.” Brian Sandoval, President of the University of Nevada wrote in his nomination, “Dr. Slonim has always answered the call, and worked with me to improve health through proactive community-based prevention, to create an exceptional healthcare system for those with acute and chronic diseases, and to care for all people in our community.” Bill Welch, President and CEO of the Nevada Hospital Association, wrote in support, “I consider Dr. Anthony Slonim to be one of the most extraordinary leaders in health care today.” Dr. Slonim is recognized nationally as a thought and opinion leader who does not accept the status quo. He is a quadruple board-certified physician by training and holds a Doctorate in Public Health and Health Policy with Fellowships in the American College of Healthcare Executives (ACHE), American Association of Physician Leaders (AAPL), and the College of Critical Care Medicine. Dr. Slonim’s holds a university appointment at the University of Nevada, Reno School of Medicine, is a highly sought after speaker on healthcare trends and leadership development, holds a Six Sigma Black Belt and is a 2-time TEDx speaker. Dr. Slonim has authored more than 120 publications, 15 textbooks, and has millions of dollars in research funding to his name. Modern Healthcare has named Dr. Slonim as one of the 50 Most Influential Leaders in Healthcare. He has been named to Becker's Hospital Review's "Physician Leaders to Know" list since 2014. Before joining Renown Health in 2014, Slonim served on the senior leadership teams for Barnabas Health in New Jersey, Carilion Clinic in Virginia and Children's National Medical Center in Washington, D.C. Slonim, who was also a registered nurse, got his medical degree from New York Medical College, served four years in the U.S. Public Service Commissioned Corps as a commander, and earned both his master's and doctoral degrees in public health and health policy from The George Washington University's Center for Health Policy Studies. About Renown Health Renown Health is a locally governed, not-for-profit integrated healthcare network serving northern Nevada, Lake Tahoe and northeast California. Renown has a long tradition and commitment to improving the care and the health of our community. For more information, visit renown.org.
Read More About Prestigious Honor Shines National Spotlight on Health Care in Nevada