Search
-
What You Need To Know About Cold Water Drowning
Northern Nevada's stunning lakes, including Lake Tahoe, with its average summer water temperature of 50 degrees, present a potential risk of hypothermia. Unlike mild 50-degree air, water at the same temperature poses severe, life-threatening risks, including rapid-onset hypothermia and drowning. Awareness of the symptoms and taking proper precautions are crucial to prevent cold-water drowning. The 4 Phases of Cold-Water Drowning 1. Cold Shock Response: This response affects breathing and happens within the first minute. An automatic gasp reflex occurs in response to rapid skin cooling. If the head goes below water, water may be breathed into the lungs, resulting in drowning. A life jacket will help keep your head above water during this critical phase. Additionally, hyperventilation, like the gasp reflex, is a response to the cold and will subside. Panic will make this worse, so the key is to control breathing. 2. Cold Incapacitation: This response occurs within the first five to 15 minutes in cold water. In order to preserve core heat, vasoconstriction takes place decreasing blood flow to the extremities to protect the vital organs. The result is a loss of movement to hands, feet, arms and legs. Unless a life jacket is being worn, the ability to stay afloat is next to impossible. 3. Hypothermia: Important to note, it can take 30 minutes or more for most adults to become hypothermic. So there’s time to take action and survive. Keeping panic at bay is critical, as you have more survival time than you think. Symptoms include: Shivering Slow and shallow breathing Confusion Drowsiness or exhaustion Slurred speech Loss of coordination Weak pulse 4. Circum-rescue Collapse: This experience can happen just before rescue and is not well understood. Symptoms range anywhere from fainting to death. Some experts believe an abrupt drop in blood pressure may cause this final stage of cold water drowning, post-rescue. Additional Safety Tips and Helpful Resources Always wear a personal flotation device as well as a wetsuit or drysuit. Your personal flotation device is the most important piece of water safety gear. Try not to panic as the first phases will subside. Controlled breathing is to staying calm. Research suggests the body can withstand the cold longer than we think. The Heat Escape Lessening Posture (HELP) is a position which helps conserve energy if you’re wearing a personal flotation device. By hugging your knees to your chest, this posture helps maintain body heat for some time.
Read More About What You Need To Know About Cold Water Drowning
-
Department Spotlight: Facilities Engineering
When an appliance or fixture stops working at home, who do you contact? If your lights stop working, you call an electrician. Is your air conditioning unit out of order? Reach out to an HVAC (heating, ventilation and air conditioning) technician. What about if your sewer drains start backing up? Time to contact a plumber. And if your fire safety equipment needs servicing? Better call a fire safety technician. Regular maintenance and repairs on the inner workings of your household are always important, and when something goes wrong, it can be distressing and inconvenient to you and everyone living with you. You feel the need to get the issue resolved as quickly as possible, right? Now imagine that those needs are magnified – to the tune of hundreds of thousands of people every year. Who could potentially take on such a monumental task? Enter: Facilities Engineering at Renown Health. Crucial to ensuring our health system performs at its peak, these team members step in to make sure every patient, team member and visitor who walks through any of our doors are able to access the facilities they need and make their time with us as comfortable – and as successful – as possible. The Silent Heroes As our care teams move heroic mountains to save lives, another set of heroes emerge behind-the-scenes. As a strong backbone of our health system, the Facilities Engineering department plays a key role in maintaining the infrastructure that supports patient care, from ensuring the HVAC systems are functioning optimally to maintaining the plumbing and electrical systems that keep the lights on and the equipment running smoothly. Renown is fortunate to have some of the most dedicated journeymen in the business. This team boasts many experts, including: Plumbers Fire Safety Technicians Craftsmen HVAC Journeymen Electricians Boiler Operators Facilities Technicians As one can imagine, every day brings on a new challenge for our Facilities team members. “Each workday is always different; it could be water, power or HVAC issues or anything in between,” said Nhil Dado, Supervisor of Facilities Services. “We are proud of the services we provide for the needs of patients and employees.” “Every day, we have a variety of equipment to work on,” added Alfred Santos, HVAC Journeyman. “Whether it’s facility upkeep, plumbing, HVAC or electrical, we want to help,” added Brian McCarty, Facilities Technician. This department works around the clock to ensure that every aspect of our hospitals and outpatient care locations meets the highest standards of safety and efficiency, from routine maintenance and equipment improvements to emergency repairs. These are huge responsibilities – all of which they perform with pride. “As an HVAC journeyman, we are responsible for making sure the air circulating in the hospital is clean,” said Christopher Bobis, HVAC Journeyman. “It is also our job to make sure the air is positive and negative in isolation rooms and ensure patients are satisfied with the temperature in their rooms.” “In addition to performing regular maintenance tasks like changing air and water filters, we complete any random work order that may come up,” added Brett Courtney, Facilities Technician. “We also recently switched out our lighting at Renown South Meadows to LED lights, which helps with energy savings.” “I overlook the boiler house equipment and coordinate the fixing of maintenance issues reported by hospital staff,” added Arnt Utnes, Boiler Operator. “We also respond to every single alarm." It’s difficult for us to imagine what our health system would be like without the Facilities team providing us with the comfortable and safe environment our patients need and deserve. Luckily, we’re never alone in our efforts to keep us running, and this department expertly leads that charge. “Along with writing down the PSI readings in the gas rooms and answering calls from dispatch and the boiler rooms, I go through all the daily work orders and complete them,” said Ken Carrillo, Facilities Technician. “It always feels good to see when we complete all the work orders for the day, especially as the next shift arrives.” “We fix, replace and dispose of pieces that are no longer in service – bottom line, we help keep the building up and running,” added Alejandro Cardenas, Craftsman. But it doesn’t stop there – Facilities Engineering is currently in the midst of creating a whole new fleet vehicle program to improve the operations of our many on-site vehicles, including trucks, forklifts and more. “I am the point of contact for all things fleet,” said Michelle Bay, Administrative Assistant. “We are building a new fleet program and working closely with leadership to move the program forward. I am involved with setting up new fleet fuel cards and can set up the program in the best interest of our internal customers while looking to the future for growth.” It’s clear that the Facilities team is indispensable to Renown. Through their expertise, professionalism and commitment to quality, they stop at nothing to keep our health system functioning at its highest level.
Read More About Department Spotlight: Facilities Engineering
-
Department Spotlight: Float Pool
Ring in the New Year and the rest of the holiday season by celebrating Renown’s Float Pool team! After coming out of the COVID-19 pandemic, it's no mystery that healthcare across the country has shifted and adapted to the growing needs and new demands of our patient populations. Renown Health is no different. As the largest not-for-profit health system in the region, we are no stranger to change, even when change presents challenges. Who do we call on when a unit needs more team members in the eleventh hour? Who can help when our patient volume spikes up with seconds to spare? This is where the Float Pool at Renown comes to the rescue. Skilled in a wide variety of healthcare specialties, from acute care nursing and critical care to care aiding and patient safety, this is the team that can seamlessly step in to provide crucial patient care to the units that need it most, whether a team is understaffed for the day or needs extra all-hands-on-deck for a specific patient or procedure. Float Pool team members are equipped to work in virtually any clinical area at Renown, making a genuine difference with every patient they encounter. A Pool of Relief Teams across Renown can breathe a sigh of relief knowing that Float Pool has their back in times of need. As the backbone of our health system, these dedicated team members possess a wealth of clinical knowledge and the ability to navigate diverse medical environments. Their flexibility allows them to fill staffing gaps and provide essential support to many different units. “We fill in the gaps of staffing to make everyone's day better,” said Patti Crepps, Critical Care Float Pool RN. “A float nurse has to be flexible and able to adapt to different situations and places – basically, ‘go with the flow.’ Patient care is basically the same all over; we make patient care possible by being familiar with all the various specialties and providing the specific care needed depending on the population we are taking care of on that shift.” “Float Pool staff members are like healthcare chameleons, transitioning between different departments,” added Shelby Riach, Acute Float Pool RN. “We incorporate flexibility, teamwork and a commitment to ensuring patients receive the best care, regardless of the setting or circumstances.” This team thrives in uncertainty; in fact, no workday is the same in Float Pool – and that’s exactly the way they like it. Working with many different teams across a multitude of specialties, these Care Aides, RNs, Critical Care Techs, Patient Safety Assistants (PSAs), Certified Nurses Assistants (CNAs) and more enjoy facing change, while they all share a goal of providing the best patient care possible. “No day looks the same; since we are the Float Pool, we are assigned a different assignment on Smart Square every day, whether it be as a care aide, a patient safety assistant, a unit clerk or patient transport,” said Melina Castenada, Care Aide. “If we are assigned as a care aide on the floor, we help assist with call lights and help with whatever nurses and CNAs may need, including feeding, transporting, walking, helping patients use the restroom, etc. When we are assigned as a PSA ‘sitter,’ we sit for the patient to help keep them safe. If we are assigned as unit clerk, we help answer phones and direct patients appropriately, file paperwork, answer call lights if needed and assist with office work.” “I love that every day is a different floor with different tasks and a different atmosphere,” added Julia Chappell, Critical Care Technician. “I find out which floor that I will be on right before my shift starts and head to the floor to find out my assignment for the day. Depending on the specialty, such as the medical-surgical floor versus an intensive care unit (ICU), my daily job tasks can vary.” When it comes to high-risk patients, who require special attention, PSAs within Float Pool step in to help. “The PSA role within Float Pool largely consists of adverse event prevention for our high-risk patients, and being a Float Pool employee allows us to work wherever we are needed,” said Dimitri Macouin, Patient Safety Assistant. “Whether it be in the emergency department, neurology or pediatrics, the PSA will be the eyes and ears for the nurses working with this patient population.” “Great strides have been made to ensure that PSAs remain vigilant and are recognized as an integral part of the patients' care team rather than 'just a sitter,’” added Karla Phillips, Patient Safety Assistant. Float Pool also oversees our Discharge Lounge, which offers patients and their families a dedicated space to reconnect and prepare for their discharge from the hospital. “The increase in utilization of the Discharge Lounge is something we are very proud of,” said Kara Abshier, Care Aide. “We assist in discharging patients from all over the hospital to help the floor and get new patients into rooms.” Every day brings a new challenge for Float Pool. As these team members wake up with uncertainty, they are ready to embrace the diverse demands of caring for patients of all ages. “The fact that Float Pool exists is amazing,” said Hannah Luccshesi, Acute Float Pool RN. “We wake up with no clue as to whether we will be working with babies, children or adults and then fill in the needs of the hospital.”
-
Department Spotlight: Security
“Safety is Number One,” isn’t just a saying – it's a fact of life, especially at Renown Health. The safety of all patients, visitors, staff and volunteers is always the top priority, and our Security Department takes that commitment seriously. This team is devoted in their efforts to provide a safe environment for all, building cooperative and proactive security processes leveraging crime prevention techniques and state-of-the-art technology. Renown Security sets the safety and well-being bar high, and they continually exceed that standard day in, day out at all of our hospitals and urgent care, primary care and lab locations. Specially Trained, Continually Present Our Security Department isn’t staffed with your run-of-the-mill Security Officers; these team members surpass security and safety expectations. Think city and state police-level standards. You read that right – many of Renown’s Security Officers come from Nevada Highway Patrol, the Washoe County and Carson City Sheriff’s Offices, the state probation and parole board and more. This team fosters specialized training in a collaborative environment. Every member of the security team has extensive training in compassion, empathy and de-escalation techniques to provide the highest levels of safety and security. They implement this training in all their daily duties, whether they are saying a simple ‘hello’ to a patient passing by or preventing harm to a staff member. Before their shift begins, the team meets to debrief meeting to discuss major incidents that occurred on the previous shift. These meetings ensure the next shift is aware of situations to be on special alert for and individuals to look out for. After, the team members head off to their assignments. “The day could be as mellow as greeting someone at the welcome table, or it could be as chaotic as de-escalating someone in distress,” said Emmanuel Fernandez-Orozco, Supervisor of Security at Renown Regional. “Regardless of the day, every experience is rewarding in its own way. The only thing that is promised is that every day will be different.” While every Security Officer has varying experiences, one aspect of their job always stays the same: they are always on alert for any potential safety issue. Even on the “slowest” days, it is important for this team to stay vigilant in order to mitigate any potential risks. There are several security programs that the team uses to keep everyone at Renown safe and secure: Renown's security operations center team (also known as dispatch) monitors all cameras in real time, with security officers patrolling parking areas 24/7. Security escorts are always available for any employee, patient or guest at every Renown location. Security Officers can escort anyone to their designated site, check surroundings for danger and monitor the person until they safely leave for their next destination. Rescue officers are available for any Renown location where an employee feels unsafe. Security maintains a strong relationship with the Reno Police Department (RPD) and assists with reporting and providing information that aids RPD in pursuing and deterring criminal activity. “In security, we are a counselor, teacher and rule enforcement officer, all rolled into one,” said Bob Stone, Supervisor of Security for Renown Health. Talk about master multitaskers! Protection is only one part of the job. Through positive and meaningful interactions with guests, patients, community and staff, regardless of where they are posted, the Security Department continually helps Renown achieve its mission of making a difference for the people they serve. Devoted Dispatch Speaking of multitasking, no one does this better than the Security Dispatch Center. Security Dispatchers are the “eagle eyes in the sky” at Renown, keeping a close watch on everything that happens within every Renown location, as well as REMSA (including Care Flight). From overlooking the many cameras around campus and administering codes over the PA system to manning the radio and phones to ensure Security Officers are dispatched quickly, our dispatch team helps ensure every safety or security issue at Renown is immediately addressed. When a call comes in, dispatchers like Jessica Fernandez, Security Dispatcher for Renown Health, go through a quick discovery process (sometimes in seconds) to figure out the details of the situation or code and what level of security is needed to assess and de-escalate. According to Jessica, the ability to prioritize is something she values in her work. “80 percent of our duties are on the phone and the radios, and we are skilled in prioritizing concerns based on the sheer volume of calls we get,” she said. Jessica and her teammates are proud of the outcomes from their calls. Their attentiveness to every nook and cranny at Renown and their quick response times to make them not only a valued partner to the Security Department but also a necessity to our health system. Your In-House De-Escalation Experts Being in a hospital environment is undoubtedly stressful for any patient, and many factors can increase these emotions. The Security Department takes these feelings seriously and never hesitates to take appropriate action to ensure the safety of everyone at Renown. With the unfortunate rise of violence against healthcare workers, especially amid the pandemic, our first-rate security team has been crucial in countering violence with specialized de-escalation techniques. The key to de-escalating, according to the Security Department, is to put yourself in the shoes of whoever you are working with. As stated by Bob Stone, the team approaches each situation by asking themselves: How would I want to be treated if I was in the same circumstance? “Being empathetic to their situation and listening to what is going on in their lives is key to re-directing them accordingly,” said Bob. “Applying real-life experience to similar circumstances can make them feel like they are not alone. Educating people on hospital policies can also help them reduce their anxieties and solve the problems.” Jhorddy Lopez, Security Officer at Renown Regional, approaches each situation with the mindset of knowing that each person’s reactions are different. “Different techniques need to be implemented every time,” said Jhorddy. “You have to use your best judgment call.” Quick and effective judgment calls are a task that the Security Department has conquered. Rosie Garcia, Security Officer at Renown Regional, knows that using your best judgment means getting both sides of the story. “Whenever I need to step in and de-escalate a situation, I first speak with whoever is attending to the patient and gather information,” said Rosie. “Then, I always get the patient’s side as well. I want to understand how they’re feeling, so both the staff member and the patient can meet in the middle and come up with a collaborative solution.” An example of the heroism and advanced de-escalation displayed by our Security Officers takes us back to last spring. In the middle of the night, a Care Flight helicopter transporting a patient and their family was about to touch down on the landing pad outside of Renown Regional. Right as the helicopter was about to land, an individual jumped over the safety barricade and onto the landing pad. Alexander Pico, a former Security Officer Lead at Renown Regional (who recently joined the Carson City Sheriff’s Department) immediately communicated with the individual to leave the area. The individual then went under the rear blade, which is the most dangerous part of the helicopter. Knowing that he had to risk his own life at this point to save another, Alexander ran around the back of the helicopter and tackled the individual, preventing catastrophic injury or even death. Steve Perkins now uses this example of a swift judgment call, which was captured on dispatch cameras, as training material for new staff. Exceptional character, compassion and emotional intelligence are the attributes that every member of the Security Department holds. As noted by Steve Perkins, these attributes “allow for a quick assessment of each situation in order to de-escalate and move towards the best possible solution." Securing the Job The Security Department at Renown is actively hiring caring, dedicated team members who are ready to jump in and perform exceptional high-risk healthcare security services for our health system. “We seek people with the right combination of ability and demeanor,” said Steve Perkins. "The training and skills development we provide result in a high caliber of success.” Every team member in the Security Department is passionate about the same thing: helping others. And in a healthcare environment, this is important. “Working a healthcare security job is far different than working any other security job,” said Jhorddy Lopez. “At a hospital, you get the chance to interact with people one-on-one. I get to experience the feeling of, ‘I can make a difference in this person’s life.’” Any interaction can change the course of a person’s day, and the Security Department embraces this fact. “I really do love helping people so much, whether it be an elderly patient who needs help with their wheelchair or a situation where I need to step in and de-escalate,” said Rosie Garcia. In order to succeed in this fast-paced department, being a collaborative team member is crucial. “A good coworker is a team player – someone that loves to work in a team atmosphere,” said Emmanuel Fernandez-Orozco. Jhorddy Lopez reiterates this, adding that “communication and trust are also extremely important. Everyone has to have great communication skills and have each other’s backs.” For people like Bob Stone, having a special connection to Renown inspires him to serve. As someone who experienced two life-saving hospital stays here, he is proud to give back to the organization that gave so much to him. “It was only natural to return to a facility I was familiar with my entire life,” said Bob. “After serving as a paramedic and transporting patients into Renown from Plumas County, I knew I was not done giving back to the community. Renown was the place to do exactly that.” All Genders Welcome A common misconception about the security field is that it is strictly a “man’s job.” In Renown’s Security Department, that couldn’t be further from the truth. As a female Security Officer, Rosie Garcia is a prime example of proving that idea wrong. As a master patroller and de-escalation expert, she ensures everything is running smoothly and that everyone feels safe at all times. “When I first started here, I knew right away that nobody that works here is biased,” said Rosie. “Everyone is equal, and I am treated as an equal in this department. I know I can do the job as well as any man." Both Rosie and her counterparts in the Security Department firmly believe that this line of work is for everyone, and they continually lift each other up and support one another. “No matter your gender, as long as you have confidence and integrity, you will do well,” adds Rosie. The Bottom Line If you are passionate about creating a secure environment to ensure patients get the care they deserve and employees receive the safety they merit, the Security Department is your team to join. “I come into work with pride,” said Jhorddy Lopez. “Knowing that I can change someone’s life – that makes me proud to work here.” “You’re in good hands with us,” closes Steve Perkins.
-
Addressing the Threat of Workplace Violence in Hospitals
In recent years, workplace violence against healthcare workers has been on the rise. According to the Occupational Safety and Health Administration (OSHA), about 75 percent of nearly 25,000 reported annual workplace assaults occur in healthcare and social service settings. Those who don’t work in healthcare may be surprised to learn that violent altercations are so common in our field. Hospital settings can create fear and stress for patients and their families. Pain, mind-altering medications and drugs, and difficult prognoses can amplify these feelings. While inappropriate responses may be understandable, violence cannot be tolerated. As the leader of a health system, protecting our employees is an issue that I take seriously. Reporting Workplace Violence Unfortunately, sometimes employees don’t report dangerous incidents fearing they might be blamed, or not realizing it’s a reportable offense. At Renown Health, we take these events seriously. We have clear, mandatory policies and protocols for reporting and investigating violent incidents. Each incident is investigated to ensure follow through and accountability. We also teach de-escalation skills to our hospital security teams, clinicians, and other frontline employees. As an added layer of protection, Renown Health has a first-rate security team that closely monitors activity on our campuses, addressing potential issues before they escalate. Our organization values our partnerships with community organizations including local law enforcement agencies like the Washoe County Sheriff’s Office and the Reno Police Department. Renown Health maintains a close relationship with these partners, and we alert them when our care teams experience an increase in violent incidents. I also recognize that workplace violence is a national problem that demands collaborative solutions. That’s why I am also proud to serve as a member of the American Hospital Association’s Hospitals Against Violence Advisory Committee. Nurses, doctors, paramedics, and frontline health workers care for us every day. It’s our responsibility to support them by ensuring they feel safe at work.
Read More About Addressing the Threat of Workplace Violence in Hospitals
-
Making Patient Safety the Priority It Deserves to Be
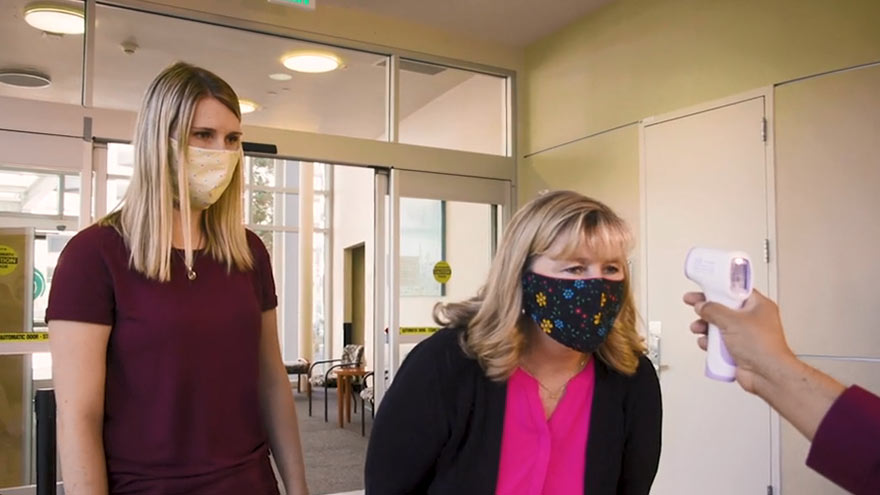
I am regularly amazed by medical advancements and innovation in the United States. However, even as we make significant progress in many areas of medicine, there is still much more work to be done in others. One such area is patient safety. What is Patient Safety? When we talk about patient safety, we are discussing how hospitals and healthcare organizations protect patients from errors, injuries and infections. Anyone can make a mistake at work, but in healthcare these mistakes can result in serious outcomes. In 1999, the Institute of Medicine released a report that estimated 98,000 deaths per year result from medical examination or treatment. The most recent study in 2013 suggested these numbers could range from 210,000 to 440,000 deaths per year. Many of these deaths result from preventable medical errors. This is inexcusable and shows how much more work our industry still needs to do to improve patient safety. Making Patient Safety a Priority Patient Safety is our number one priority at Renown Health. We dedicate a lot of time to establishing, reviewing, and revising our processes to prevent errors. Despite the obvious importance of patient safety, this issue is largely left to individual hospitals and health systems to manage. There is a surprising lack of national attention around this truly important issue. However, a silver lining of the COVID-19 pandemic is that it is igniting interest in hygiene and infection prevention. Patients want to learn more about the processes that are in place to prevent the spread of infections. In addition to the many protocols that guide our treatment of injuries and illness, Renown Health has implemented the following measures to prevent the spread of communicable diseases: Requiring everyone entering Renown sites to wear a mask or face covering. Establishing new processes to help patients and visitors practice social distancing. Limiting the number of visitors in our facilities. Screening all employees and patients for symptoms. Enhancing our already-thorough cleaning and disinfection processes. I hope patient safety and infection prevention remain in the national spotlight long after the COVID-19 pandemic has ended. The healthcare industry must come together to develop stronger systems and regulations to minimize preventable medical errors. We have a responsibility to our patients to do better.
Read More About Making Patient Safety the Priority It Deserves to Be


.png?rev=fcd27802b7604a96bf1056b050ef90c5)