Search
Results for 'what is an'
Clear-
Recognizing World Lymphedema Day
To recognize World Lymphedema Day, Katherine Bunker, Physical Therapist and Certified Lymphedema Therapist (PT, DPT, CLT) at Renown, shares her experience helping those with lymphedema and lymphatic disease thrive in their daily lives. Each year, World Lymphedema Day continues to be an advocate-driven celebration and global education opportunity on what it means to live with lymphedema and lymphatic disease. We explore why this cause deserves global recognition each year on March 6 below. Types of Lymphedema Lymphedema is an abnormal collection of protein-rich fluid that causes swelling just beneath the skin. The fluid, which is filtered through the lymph nodes, makes up a network of tissues that help the body get rid of toxins, waste and other unwanted substances. According to Katherine Bunker, PT, DPT, CLT at Renown Health, this collection of fluid causes swelling, usually in the arms or legs, but can happen in other areas too. It can also cause discomfort, restricted movement and may increase the risk of infections.
-
Prostate Cancer: Symptoms, Treatments and Screenings
Did you know: More than 2.9 million men in the United States who have been diagnosed with prostate cancer at some point are still alive today. Prostate cancer is common, but also treatable, especially when caught early. Dr. Michael Hardacre of the Renown Institute for Cancer explains. With the exception of skin cancer, prostate cancer is the most commonly diagnosed form of cancer in American men. In fact, the American Cancer Society offers these key statistics: About 1 man in 9 will be diagnosed with prostate cancer during his lifetime. Prostate cancer develops mainly in older men and in African-American men. About 6 cases in 10 are diagnosed in men aged 65 or older, and it is rare before age 40. The average age at the time of diagnosis is about 66. The good news: This form of cancer is very treatable when also detected early. Michael Hardacre, MD, radiation oncologist with Renown Institute for Cancer, is here to explain more about prostate cancer screenings and their role in early detection. What is the prostate? The prostate is a gland that only males have, and it makes part of the seminal fluid. Prostate cancer begins when the cells in the prostate gland start growing uncontrollably due to a change in the cell’s genes. Researchers are working to find what leads to the disease. Certain types of prostate cancer are hereditary, or passed on through genes. However, most types of prostate cancer are acquired and developed later in life. What are some of the signs of prostate cancer? Common signs of prostate cancer include: Frequent urination Weak urine flow Painful urination or inability to urinate Blood in urine or semen Painful ejaculation Erectile dysfunction If you notice any of these signs, talk with your primary care doctor. Although it may be intimidating to talk about any of these signs or symptoms, the earlier prostate cancer is detected, the better the options for treatment. How can you screen for or detect prostate cancer? The good news is that prostate cancer can often be found before symptoms appear, because screening is as simple as a blood test. Your doctor will look for levels of a prostate-specific antigen in the blood. If the results come back with anything concerning, then additional testing would be recommended. A transrectal ultrasound can also be used, which is usually painless and only takes about 10 minutes to complete. This exam gives the doctor an image of the prostate to measure its size, which can help determine the density of the prostate-specific antigen. If this test comes back with any suspicious results, then your doctor may recommend a biopsy. What are the treatment options? Depending on each case, treatment options for men with prostate cancer might include: Watchful waiting or active surveillance Surgery Radiation therapy Cryotherapy (cryosurgery) Hormone therapy Chemotherapy Vaccine treatment Bone-directed treatment It’s important to discuss all of the treatment option with your doctors, including goals and possible side effects, to help make the decision that best fits your needs. Some important things to consider when choosing a treatment option also include: The stage and grade of your cancer Your age and also your expected life span Any other serious health conditions you have Your feelings (and your doctor’s opinion) about the need to treat the cancer right away The likelihood that treatment will cure your cancer (or help in some other way) Your feelings about the possible side effects from each treatment Renown Institute for Cancer | 775-982-4000 At the Renown Health Institute for Cancer, our experienced team provides the support and care to maintain the highest quality of life and then achieve the best possible outcome, all in one location that’s close to home. Our dedicated team, clinical expertise and also advanced treatment options allow us to tailor care to each patient. Learn about: Our Team Cancers We Treat Screening and Prevention Treatment Options
Read More About Prostate Cancer: Symptoms, Treatments and Screenings
-
From Renown NICU Nurse to NICU Mom: Mariah DaSilva’s Inspiring Journey
Located on the 5th floor of the Tahoe Tower, Renown’s newly updated Level III Neonatal Intensive Care Unit (NICU) is decorated with colorful artwork on the walls, the lights dim for the newborns resting, and parents conversing next to the bassinet with nurses on their baby’s journey to health. In the quiet, shuffling hallways stands Mariah DaSilva, a Renown NICU Nurse, whose own birth story showed her true compassion and professional dedication to what it means to care for the tiniest and most vulnerable patients. From the Medical Floor to the NICU Mariah started her nursing career on the medical floor at Renown; however, after a year, she was excited to see her dream job open in the NICU and helping to provide compassionate care for the most fragile patients. “I’ve always known that I wanted to work with babies so being a NICU nurse was a dream of mine,” said Mariah. “I truly love what I do, and I can’t imagine being anywhere else than the NICU.” A high-stakes environment, the NICU is where babies are transferred to after birth when they require medical intervention. They care for babies as young as 23 weeks gestation, up to full-term babies. Any babies born less than 35 weeks are automatically admitted into the NICU for treatment. Other than prematurity, babies can be admitted to the NICU for respiratory distress, low blood sugar (hypoglycemia), cardiac anomalies, birth defects, seizures and other medical conditions that need treatment or assessment. A Day in the NICU: The Heart of Care A typical day for Mariah starts with reviewing her assignments and receiving a detailed report from the night shift. Preparing for the day involves scrubbing in and wiping down patient care areas to maintain a clean environment. Once everything is set, she begins a series of scheduled care tasks, which include performing assessments, feeding, changing diapers and facilitating parent involvement in their baby’s care “There are so many exciting ‘firsts’ that happen in the NICU; parents holding their baby for the first time, parents' first time changing their baby’s diaper, bathing their baby for the first time, first time breast-feeding or bottle-feeding, the baby’s first time taking a full bottle, watching a baby breathe on their own without any respiratory support, etc.,” said Mariah. “There are so many big milestones that happen in the NICU that I am so incredibly lucky to be a part of.” The NICU nurses work closely with neonatologists, nurse practitioners, respiratory therapists, speech therapists, physical therapists, occupational therapists and other specialists to deliver comprehensive care. This teamwork and collaboration ensure that each baby receives the best care possible for their health journey. Mariah shared a reflection on her team: “Our NICU team is amazing. Being a part of a team that is so compassionate and collaborative is amazing. We all work closely together to ensure we’re providing the best care possible for every single baby that comes to the NICU. We are all very protective of the babies that we care for in the NICU and truly want the best outcomes for them and their families. Taking care of such a vulnerable population comes with a lot of responsibility and we take pride in what we do each day.” As with all healthcare professionals, NICU nurses require immense strength and compassion to care for the youngest patients in a highly sensitive environment. “More often than not, we have really good days in the NICU, but we also have really hard days that affect every single person in the NICU,” said Mariah. “The loss of a baby, delivering bad news to a parent, an extended NICU stay and a baby withdrawing from drugs are all situations that we unfortunately deal with in the NICU. These situations are all very challenging, but we have to stay strong for the babies and their families.”
Read More About From Renown NICU Nurse to NICU Mom: Mariah DaSilva’s Inspiring Journey
-
Perseverance and Physical Therapy Help UNR Student Walk Again
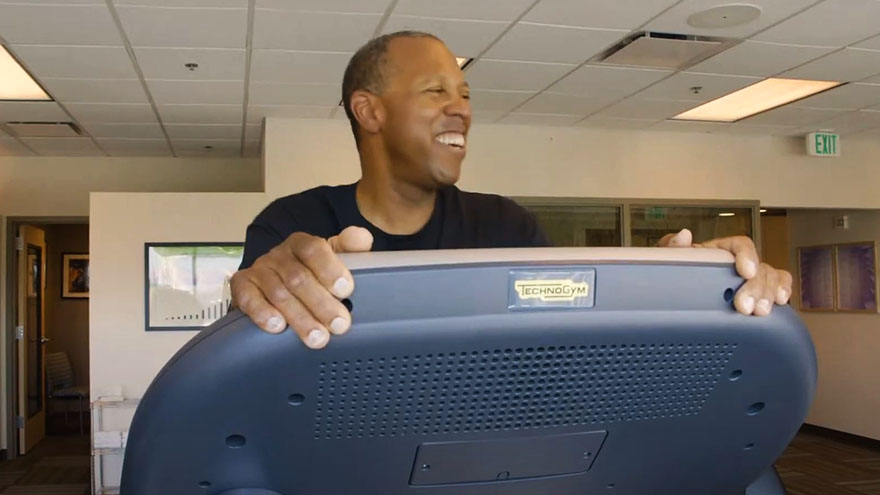
University of Nevada, Reno student Khoa Le was paralyzed in 2010 after a longboarding accident. Through physical therapy, a positive attitude and sheer will, Le is walking again. This weekend, Le will walk across the commencement stage to accept his college diploma. “Walking around on my own power is just the greatest feeling,” says Khoa Le, a senior at the University of Nevada, Reno. Just after finishing summer school at the university in July 2010, his whole life changed within seconds after stepping on a longboard skateboard for the first time. He lost control of the board and hit the curb, causing paralysis on the left side of his body. His journey to recovery began at Renown Health Physical Therapy & Rehab. His physical therapist, Dina Barry, says he never complained once in four years. “I started seeing Khoa in April 2011, and we worked for four years together,” says Barry, a lead physical therapist at Renown. “Everything I’ve ever asked him to do, he does. Le is a hard worker, is continuously optimistic and smiling, and I think that is why he’s accomplished what he has.” Le plans to pursue a career as an information systems manager.
Read More About Perseverance and Physical Therapy Help UNR Student Walk Again
-
Going the Distance to Get Heart Healthy
After having a heart attack, a Mammoth resident travels to Reno to complete rehab. He’s already lost 15 pounds and gained a healthier outlook on life. Eric Smith travels from his home in Mammoth Lakes, Calif., to Reno twice a week to participate in Renown Health’s Healthy Heart Program. “Living in Mammoth, it’s a three hour drive for me up here. Well, it’s my life or it’s a drive,” says Healthy Heart Program participant Eric Smith. The Mammoth Lakes, Calif., resident travels to Reno twice a week to participate in the 72-session program. which includes heart-healthy classes, exercise sessions and cooking demonstrations. “The cardiac rehab program here is excellent,” Smith says. “It is the only program that I am aware of that combines nutrition and exercise together. What’s the point of exercising to get your heart strong if you are still eating poorly and not educating yourself on that?” Smith’s heart issues began when he was 46-years-old. He received an angioplasty, which is a stent to hold a coronary artery open. Two years later, Smith had a heart attack and was flown to Renown Regional Medical Center for emergency bypass surgery on four arteries to allow blood to flow to his heart more freely. An avid skier, ski racing coach and tile setter, Smith admits that it is sometimes difficult to eat right when you’re on the go in a tourist town. Since starting the cardiac rehab program, Smith says he is feeling more optimistic on making lasting lifestyle changes after meeting other people who are going through the same challenges, like food cravings and trying to get stronger. “The big thing is getting educated on food,” says Smith, who has swapped out heavy breakfasts for whole grains and fruit, and steak dinners for baked fish. In just a few months of starting the program, Smith lost 15 pounds. He looks forward to passing along what he’s learned to his friends. “Everybody benefits from this program, especially if you have experienced a heart attack,” Smith says. “But if you don’t have those issues, you can still get the benefits from eating healthier.”
-
Building a Better Birth Team
Giving birth expends as much energy as running a marathon. And just like you would only run a marathon with training beforehand, there are exercises you can do to prepare for birth. But instead of a coach, you'll have your birth team. Your birth team exists to help you navigate pregnancy and labor and support your choices. Let's say you've never put together a birth team before and are wondering where to start. Today we'll go over the three main positions to fill for your birth team's starting lineup. Birthing Person The birthing person is the leader of the team. After all, you can't have a birth team without someone giving birth. This person could be the baby's mother, gestational surrogate, birth parent before adoption, a transgender father or a non-binary parent. If you are not the birthing person, don't presume to know what the ideal labor and birth circumstances should be. And if you are the birthing person, don't allow anyone else to tell you what you want. This is your body and your birth; you are the boss in the birth room. Doula No birth team is complete without a doula, and although doulas have increased in popularity lately, many people still don't know what a doula is. Simply put, a doula is a birth professional – not a medical provider – who offers emotional, physical and informational support during pregnancy, labor and beyond. Most doulas' services include at least one prenatal visit and one postpartum visit, as well as continuous care throughout active labor. Some doulas provide more than one prenatal/postpartum visit, so be sure to ask what is included in their fee. Even if you have a partner who will support you during labor, studies have shown that a doula can significantly increase your likelihood of a positive birth outcome. Even the most supportive partner needs to rest, and a doula can ensure that you still get the care you need while your partner gets a break. Midwife or Obstetrician Finally, you'll want to choose the medical professional who will attend your birth. Many folks choose to give birth with the OB/GYN who does their annual check-ups, but there are many reasons someone might choose a different provider for their birth. The first step to finding the best attending provider for your birth is to decide which model of care aligns closest to your values and goals: the Midwifery Model of Care or the Medical Model of Care. .tg {border-collapse:collapse;border-spacing:0;} .tg td{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; overflow:hidden;padding:10px 5px;word-break:normal;} .tg th{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; font-weight:normal;overflow:hidden;padding:10px 5px;word-break:normal;} .tg .tg-gqvw{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-weight:bold; text-align:left;vertical-align:top} .tg .tg-8vim{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-size:18px; font-weight:bold;text-align:left;vertical-align:top} .tg .tg-qm8j{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;text-align:left; vertical-align:top} .tg {border-collapse:collapse;border-spacing:0;} .tg td{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; overflow:hidden;padding:10px 5px;word-break:normal;} .tg th{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; font-weight:normal;overflow:hidden;padding:10px 5px;word-break:normal;} .tg .tg-gqvw{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-weight:bold; text-align:left;vertical-align:top} .tg .tg-8vim{background-color:#ffffff;color:#56266d;font-family:Arial, Helvetica, sans-serif !important;font-size:18px; font-weight:bold;text-align:left;vertical-align:top} .tg .tg-2rvk{background-color:#ffffff;color:#000000;font-family:Arial, Helvetica, sans-serif !important;text-align:left; vertical-align:top} Midwifery Model of Care Medical Model of Care Philosophy Birth is physiological. Birth is potentially pathological. Interventions Medical interventions can cause more complications, and therefore are only used as needed. Medical interventions should be used, even in non-emergency situations and sometimes as preventative measures. Decisions Birthing person is the key decision maker. Medical professional is the key decision maker. Provider’s Role Providers monitor labor and will intervene or transfer to hospital if needed. Providers assess and control the birthing process.
-
How to Get Your Kids to Sleep, Screen-Free
If you’re a parent, you’ve probably been there — the sometimes-nightly struggle to get your little ones off to bed. Elaina Lantrip, an APRN with Renown Pediatrics, offers some tips and explains how your child’s electronics may be getting in the way of a good night’s sleep. These days, kids are consuming media from a very early age on all types of devices — from tablets and phones to TVs. While they can benefit from some media use, it can have a negative impact on bedtime. We asked Elaina Lantrip, an advanced nurse practitioner with Renown Pediatrics, for some advice on downloading a better bedtime routine. What are the most important practices for parents to establish for their children’s bedtime routines? I often have parents tell me that their child won’t go to bed — or to sleep. Parents frequently ask for tips on bedtime routines that work. My first question is whether their regular bedtime routine involves television, iPad, tablet, phone or anything with a screen. It’s very important that bedtime includes a bath, reading a story, talking, singing and bonding with young ones, rather than using any devices. Why shouldn’t children have a device at bedtime? A growing body of research supports that screen time at bedtime contributes to delays in a child’s falling to sleep; overall inability to reach the important REM, or deep sleep; waking up during the night; nightmares and night terrors. For older youth, engaging with social media before bedtime can bring up stresses, emotions and relationship issues with peers that don’t exactly create peaceful bedtime thoughts. Bedtime should be a screen-free, stress-free, peaceful time of day. It’s a great time for parents to promote self-esteem, talk through things going on in the child’s life, to encourage and build them up. Children grow up fast — bedtime is a great the opportunity with younger children to cuddle up and read a story or sing a lullaby. What are other major considerations in making bedtime smooth and relaxing for kids and their parents? Another factor that contributes to positive sleep habits includes children getting enough activity during the the day so they’re genuinely tired at night. Also helpful are ambient noise makers, peaceful music, avoiding sugar two hours prior to bedtime, consistency in bedtime routine, comfortable pajamas and comfortable temperature in the home. Is it important to keep the child’s bedroom dark? Dimming the lights is important, regardless of the time of year. This is another reason to ban screens, as they emit light that stimulates wakefulness.
-
Heart Failure Risks and Expecting the Unexpected
For the average person, detecting the signs of heart failure can be tricky, especially since people can look fairly healthy and have few symptoms. We asked Christopher Rowan, M.D., of the Renown Institute for Heart & Vascular Health, to answer our most pressing questions about heart failure. Even with more technology in medicine and a greater awareness about health today, the Centers for Disease Control and Prevention still reports that one in every four U.S. deaths is caused by heart disease. The real tragedy of heart-related deaths is that they are both common and preventable. “Heart failure can have many forms that are seen in anyone at any age," says Christopher Rowan, MD, with Renown Institute for Heart & Vascular Health. "As many forms as it has, it can also have as many causes. Although the symptoms of heart failure are numerous, people can look mostly healthy and have relatively few symptoms.” We sat down with Dr. Rowan to ask some common questions about heart failure. How can I tell if I have heart failure? What are some sure signs? "The signs and symptoms of heart failure are numerous, but the most common ones are shortness of breath when trying to walk (which differs from somebody’s normal pattern); progressive swelling in the feet, legs and ankles that does not disappear overnight; and waking up at night due to shortness of breath or waking up more than normal to urinate," Dr. Rowan says. Can heart failure be cured? "The treatment of heart failure depends on its primary cause," Dr. Rowan says. "Various forms of heart failure can be cured; however, the person is always at risk for recurrence. Some forms of heart failure have no cure but can be managed and stabilized and people can live a relatively normal life for years." What can I do to prevent heart failure? "To prevent the onset of heart failure, know your risk factors, including high blood pressure, diabetes, smoking and an unhealthy lifestyle," Dr. Rowan says. "If you have any of these risk factors, work to get them under good control and stop smoking. If you are overweight, start a daily routine where you walk at least 45 minutes per day, 5 days per week. Walking is the best exercise for your cardiovascular health." To learn more, visit the Heart Failure Program at the Renown Institute for Heart & Vascular Health. We want to hear your story! If you or a friend have been treated for a heart condition at Renown Health and are interested in chatting with us about your experience, please email your contact information to support@renown.org so we can follow up.
Read More About Heart Failure Risks and Expecting the Unexpected
-
Baby's Ears and Altitude Changes
One of the best things about living in the Reno area is the beautiful mountain range that surrounds our city. Many families take advantage of the activities the mountains have to offer or travel over them to visit friends and family in neighboring areas. However, for parents of infants there is often angst over your baby’s ears and altitude changes and the associated potential for ear pain and/or “popping.” Fortunately, there are things you can do to protect your infant’s ears the next time you drive over the mountain or hop on a plane with your little one. Baby’s Ears and Altitude Changes: What Causes Them to “Pop” The simple answer is pressure. The problem originates in the middle ear where there is an air pocket that is vulnerable to changes in pressure. The Eustachian tube, which runs behind the nose to the middle ear, is constantly absorbing and resupplying air to this pocket to keep it balanced. When the pressure is not balanced, your ears feel “clogged” or like they need to “pop.” In some cases this sensation can cause significant ear pain and even temporary hearing loss. Rapid changes in elevation or altitude, like driving over a mountain, or ascending or descending on an airplane, can cause rapid changes in pressure. In order to avoid problems, the Eustachian tube needs to open widely and frequently to equalize those pressure changes. The problem often intensifies during descents as you go from an area of lower atmospheric pressure to an area of higher atmospheric pressure. This is why you hear babies screaming on planes during descent or why your infant is wailing in the car seat as you head down the mountain. What can you do to make it a more comfortable trip for your child? First, be prepared. Babies cannot intentionally “pop” their ears like adults can, but we can help them by encouraging them to swallow. Offer your baby a pacifier or bottle while making ascents and descents. If possible, it may be helpful to have an adult ride in the back seat with baby if you’re in the car to ensure this can happen. Don’t let your baby sleep during descent on a plane. Help your little traveler out by offering him or her a pacifier during this process, as descent is the most likely time for pain associated with altitude changes. If your baby is congested prior to travel involving altitude changes, seek the advice of your pediatrician since they may have other solutions, including medications such as decongestants. If you return from a trip and notice your infant is still fussy and uncomfortable, contact your child’s doctor for a thorough ear evaluation. Safe travels!
-
Club Member with a Grand Tale
Renown’s Sterling Silver Club is honored to feature one of our more than 9,000 members each season. We thank Judith for sharing her inspirational story and all of our members for leading healthy, happy lives that inspire us all. Mother, grandmother and eventually great-grandmother is the expected title progression as families grow and babies have babies. “Grand” and “great” usually imply roles and responsibilities have shifted from daily child-rearing duties to those of a doting grandparent – that is, unless you decide to do it all over again. At the age of 61, that’s exactly what featured Sterling Silver Club member, Judith, decided to do when she adopted four of her great-grandchildren. At the time, Alicia, Adrianna and Joey were all under five and Giancarlo, the youngest, was just a baby. “At the adoption hearing, the judge was concerned how stressful it would be for me to raise four children in my late 70s and early 80s,” recalls Judith. “But I told him I had raised my own four children and then three grandchildren for a number of years and that it would be far more stressful for me to have my great-grandchildren separated from each other and me, possibly forever. I knew I could handle the stress of raising them no matter my age, but I couldn’t survive the stress of losing them.” “That was when Giancarlo started getting fidgety,” she continues. “So I raised up his little shirt and blew a raspberry on his tummy which made him giggle and settle down. Seeing that, the judge told the recorder to “put that move in the record” and agreed I was capable of caring for my little ones.” Years later, Judith has come to realize that her great-grandchildren also want to be there to care for her. “Giancarlo always makes me smile,” says Judith. “Once during a stay in the hospital, I was awoken at 3 a.m. for blood work and found him sitting next to my bed watching the oxygen count – he was 10 years old at the time.” “The nurse asked him why he was awake and he said he heard her say the count shouldn’t go below 88, so he was watching to save me if it did,” Judith explains. “The nurse reassured him that she was also watching the count at her desk and he didn’t need to worry. Then Giancarlo looked her square in the eye and told her if it went below 88 to wake him up because he loved me and didn’t want to lose me.” “He is still my sunshine,” Judith smiles. “And I have never regretted my decision.” Work & Play For 20 years, Judith worked at Truckee Meadows Community College (TMCC), first as an administrative assistant for the police academy before moving to a position in the president’s office. There she worked with the TMCC Foundation and on TMCC projects to raise capital funds for new buildings, off-site campuses, scholarships, college programs and more. “It felt wonderful to be able to notify a student that they had received a scholarship or tell a department that they had received the funds to purchase needed equipment for their program,” recalls Judith. For fun these days, Judith still enjoys doing something she did as a teenager: playing pool. “My mother taught me to play pool in my dad’s pool room/teen hangout space in my early 20s and I’m just getting back into the game by taking lessons to help remind me what I was taught,” says Judith. “I grew up in a small, country town on the Ohio River and my mother could beat almost all of the boys in the county. I would love to be able to emulate her ability in the game.” Judith also enjoys reading, watching Hallmark movies or Warriors basketball games, walking in nature, playing “competitive” shuffleboard with friends, all genres of music – and dancing! In fact, she’s currently taking dance lessons to learn a few new steps. Always Good for a Laugh “My great-grandchildren and I laugh a lot when I try to teach them the stroll, twist, mashed potato and old-fashioned, rock-‘n’-roll dancing,” admits Judith. “But we laugh even harder when they try to teach me their dance moves!” Faith in What Matters Faith is something Judith celebrates and embraces for herself and others. “I truly believe that we are placed on earth exactly where God feels we are needed and that we are here to help each other through life, not to accumulate material goods for ourselves,” says Judith. “I feel deep satisfaction when I can help others either through just listening to them, advising them, helping them with specific needs or simply giving a smile to a stranger. To me, giving a smile or a helping hand to someone is like skipping a rock across the water – the ripples go on and on.” Then she adds, “And raising my great-grandchildren to be able to have wonderful lives full of love and happiness and closeness to God is the greatest gift I could give them.” Club Talk So what does Judith appreciate most about being a member of the Sterling Silver Club? She says it’s the opportunity to just – talk. “I fully enjoyed my initial interaction with the club and other club members at the Roaring Twenties dinner dance event,” remembers Judith. “I sat at a table with the nicest ladies and had great conversations with adults and danced with one of the instructors. When you are raising four teenagers who sometimes seem to speak an entirely different language, it’s refreshing to meet and speak with others your own age.” Pictures of some of the popular Sterling Silver Club events are featured here. Judith finds club events that bring her joy. “I also like the cooking classes and recently went on a walking tour of Oxbow Park, which was very peaceful.” What advice does Judith have to help other members live their best and fullest lives? “On a wet December morning 50 years ago,” Judith begins, “a truck coming around a curve on a country road slid into me and that split second could have made all the difference in the world to me. But God was with me and I survived, which no one expected.” “You never know when that one second that could change everything might happen, so make the most of all of your seconds,” she advises. “Do what you love with those you love. My family means the world to me and I try to think about how my decisions will reflect on the memory I will leave behind for them.” Then Judith thoughtfully adds, “I want them to remember that I truly loved them and always did my best to let them know that.”
-
Powerlifting through MS Diagnosis
When Tabitha Cox received a diagnosis of multiple sclerosis (MS), she was in shock, denial and felt that she was too strong for something like this to be happening to her. As the disease progressed, Tabitha realized she needed to do what she could to stay as healthy as possible. “I heard, ‘You have a quarter-size lesion on your brain,'” recalls Tabitha Cox. “At that moment, that was literally all I heard come out of her mouth.” Tabitha’s official diagnosis was multiple sclerosis (MS), an unpredictable, often disabling disease of the central nervous system that slowly debilitated her mom. “I was numb,” says Tabitha. After her diagnosis, Tabitha went on with her life as if the disease was nothing more than a doctor’s diagnosis. However two years later, Tabitha realized something wasn’t right and sought care at Renown Institute for Neurosciences – Brain and Nerve Care. Her form of MS was aggressive, and her doctor recommended treatment right away.
-
Meditation: Give Yourself the Gift of Inner Peace
As we enter the holiday season, many of us are beginning to plan and partake in festivities such as shopping, cooking, baking, holiday parties and family gatherings. While the holidays often bring joy and cheer, the hustle and bustle can also lead to fatigue, stress, anxiety and sometimes depression. To avoid holiday burnout, it’s important to find ways to care for yourself mentally and physically. Galen Gorelangton, Renown's Spiritual Center Volunteer, discusses how yoga and meditation can benefit you. What is yoga and meditation? Yoga is defined as performing a series of postures and controlled breathing exercises to promote a more flexible body and a calm mind. As you move through poses that require balance and concentration, you're encouraged to focus less on your busy day and more on the moment. Meditation involves focusing or clearing your mind using a combination of mental and physical techniques. While there are many different types of meditation and yoga practices, they both share similar benefits including: Reduced stress Lower blood pressure Decreased anxiety and depression Increased energy Better sleep Lower inflammation and pain levels Improved strength, balance and flexibility Better focus and concentration And much more!
Read More About Meditation: Give Yourself the Gift of Inner Peace