Search
Results for 'find a primary care physician'
Clear-
Dry Weather and Your Health – What to Know
Dry weather – as northern Nevadans we know it well. Of course this doesn’t mean we’re not affected by its health impact whether you’re new to the area or are a native. Stephanie Stutz, DO, a Renown Medical Group doctor specializing in family medicine, explains how to live comfortably in the high desert. Have you noticed dry skin, itchy eyes or more bloody noses? If you call northern Nevada home, you’re probably no stranger to these problems. “We get a lot of questions from people wanting to know, ‘what can I do to prevent things from happening from the dry weather?’” says Dr. Stutz. “We do have a dry climate, and obviously in the summertime you notice it more than in the winter, so we look at things like dry skin, dry eyes and dry nose.” It generally takes about two weeks to become used to the change in climate. Dry Weather Health Tips Fortunately, there are some easy things you can do to reduce your discomfort in dry weather. Dry skin. “If you have dry skin, use a lotion without perfumes so it won’t increase the potential for drying your skin out,” recommends Dr. Stutz. For example, one home remedy for extremely dry skin (or for those with thinner skin) is cocoa butter. “It’s thicker so it goes under the skin and takes more time to absorb. As a result, you get a much more long-lasting effect.” Dr. Stutz adds. “You can also add lavender essential oil to your cocoa butter to help you sleep at night.” Dry and itchy eyes. “Use eye drops on a regular basis and keep them with you. I recommend people have a couple of bottles – one at home and one in their bag,” Dr. Stutz suggests. Dry nose. “Overall one of the best things to use is a simple nasal wash,” she says. “You can get it over the counter; it’s a saline nasal wash. Use it a couple of times each day and it can be extremely helpful. In particular, gets up into the sinuses and clears them of any pollen or residue in there.” Dry Weather Nosebleed Advice In our dry climate, you may also notice more allergies and nosebleeds. Dr. Stutz cautions, “Surely the dry air can make your allergies much worse. It can create much more irritation, pain and pressure, particularly in the nose and sinuses.” Again, Dr. Stutz recommends using a nasal wash to remove discomfort. Using a nasal wash two to three times a day can also help prevent nosebleeds. “And if you’re someone who has severe or chronic nosebleeds, you can put a little bit of Vaseline along the inside of your nose to create a moisture barrier”. Dry Weather Medication Advice In addition to allergy and nosebleed sufferers, people on certain medications may be at greater risk for symptoms in our dry climate. “The medications you are on can make you much more susceptible to drying out and becoming slightly dehydrated,” Dr. Stutz warns. For this reason discuss all of your medications with your doctor. Specifically, see if you can time them throughout the day or look at changing the dosage. Should I Get a Humidifier? Given our year-round dry weather, you may want to purchase a humidifier to help ease your symptoms. But there are some things you should know first. “You have to be careful with humidifiers as there are pros and cons,” states Dr. Stutz. “The small tabletop humidifiers are not beneficial. You need to get one covering a huge amount of square footage and holding approximately 10 to 30 gallons of water to help your home. On the negative side, if you’re not maintaining it on a regular basis, it will hold on to mold and other allergens. So the next time you turn it on, you’re actually putting that back into the air.” Do I Need to Go to the Doctor? To be sure, it’s important to know yourself and your family. If this is something you experience each year, you can try over-the-counter medications. “But remember, there’s always the caution if you’re on prescription medications,” Dr. Stutz explains. “If you are on chronic prescriptions, come in to get evaluated just to make sure you’re not using anything which interferes with your medications.” Not Just a Summer Problem As the temperatures drop, remember this isn’t just a seasonal issue here in the Reno-Tahoe area. During the winter months, our dry climate combined with cold temperatures and heaters can still cause dry skin, aggravated sinuses and even itchy eyes. So use these helpful dry weather tips all year. Comprehensive Primary Care Renown Medical Group primary care physicians provide comprehensive primary care by appointment. Doctors coordinate each patient’s medical care including checkups, immunizations, referrals to specialists, lab work, X-ray & imaging and hospital admissions. Find a Doctor
-
Why Am I So Tired? 9 Reasons for Your Chronic Exhaustion
Do you find yourself struggling to stay awake during the day or having no energy? You’re not alone. Whether you’re a full-time employee, a student or retiree, that “I’m tired” feeling comes in all shapes and sizes. What’s even more frustrating is not knowing the source of your exhaustion. Dr. Brandon Flores, a sleep medicine physician with Renown Medical Group, breaks down nine key reasons why you may be feeling so fatigued. You did not get enough sleep, or your quality of sleep is poor. This may seem obvious, but in today’s “rise and grind” culture, sleep can be considered a luxury rather than what it really is: a necessity. Ensuring you get adequate hours of sleep between 6-9 hours and quality sleep is essential. You may not be breathing well during sleep. Interruptions to your breathing, such as snoring, can decrease airflow at night causing your sleep to be less restorative. This is often due to Obstructive Sleep Apnea (OSA). OSA can lead to daytime fatigue and sleepiness and can also impact other chronic health conditions, such as hypertension, diabetes, acid reflux, migraines and heart rhythm. You are not getting enough regular exercise, or you are exercising too much. Incorporating at least 30 minutes a day of physical activity can help keep you energized throughout the day. It has also been shown to increase deep slow wave sleep, which is often associated with feeling rested. On the other hand, getting too much exercise can tire you out more easily and heighten stress levels. You drink too much caffeine. This one may seem counterintuitive – caffeine is supposed to keep you awake, right? Well, overdoing it with your favorite coffee or soda could affect your sleep quality. Pay attention to your caffeine limits and have a cut-off time, as most caffeine should not be consumed past noon. You have a food allergy or intolerance. If you find yourself feeling especially tired after eating a lot of a certain food, you could have an allergy or intolerance to it – and vice versa. Consider speaking with your primary care provider (PCP) about a food allergy test or being referred to an allergist. You’re drinking too many alcoholic beverages. Alcohol is a depressant, which as the word implies, can make you feel especially tired during the day. It can also affect your breathing at night and disrupt your sleep cycle. Cutting back on alcoholic drinks may be beneficial to your overall health. You are anemic. This is the leading cause of fatigue in women but can affect people of all genders. It can be associated with low iron. Eating foods high in iron, including leafy greens and many different meats, can help your iron levels. A blood test ordered by your PCP can help you understand if you are iron deficient. You are experiencing depression or anxiety. Emotional exhaustion can be just as taxing as physical exhaustion. Prolonged feelings of sadness, hopelessness, nervousness or panic can be signs and symptoms of depression or anxiety. Speak with your provider about the many resources available to help you. You have an underactive thyroid. Feeling fatigued can also be a symptom of hypothyroidism, which affects your metabolism and energy levels. Medication can help get your thyroid back to normal. Your PCP can order a blood test to determine your thyroid levels. If you experience severe exhaustion that lasts six months or longer, worsens after physical or mental exertion and does not get better after resting, it could be a sign of myalgic encephalomyelitis, otherwise known as chronic fatigue syndrome (CFS). This is a diagnosis of exclusion, and other causes must be ruled out. While there are no tests that detect CFS, your provider can order blood and urine tests to rule out other causes of your fatigue and help develop a care plan. © Africa Images via Canva.com
Read More About Why Am I So Tired? 9 Reasons for Your Chronic Exhaustion
-
3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
Ensuring a healthier and more inclusive future for LGBTQIA+ children and teens is of utmost importance to health systems in our community, especially Renown. Supporting the physical and mental health of youth in this community is key to those efforts, especially as they face unique challenges in terms of identity acceptance and social integration. Dr. Caroline Barangan, Adolescent Medicine Physician with Renown Children’s Pediatric Specialty Care, discusses what you as a parent, caregiver, friend or support system can do to be a safe space for children and teens who identify as LGBTQIA+. 1. Create a Safe Space at Home The most important action you can take for your LGBTQIA+ teen or child is to accept and support them for who they are, regardless of how they identify. “Being a teenager is already difficult enough, especially within the LGBTQIA+ community, which puts them at risk of being stigmatized, rejected and targets for bullying,” said Dr. Barangan. Your supportive words and actions can make a huge difference as a profound expression of love and understanding. Being patient and willing to learn are the foundations to a healthy and loving relationship with your LGBTQIA+ teen or child. 2. Encourage Regular Check-Ups with a Primary Care Provider (PCP) Establishing your child or teen with a PCP is not only important when an illness occurs but also for annual preventative visits and regular check-ups. “A primary care provider can screen for high-risk behaviors that would put a patient’s health in jeopardy, such as sexual experience, substance use, suicidality and self-harm,” said. Dr Barangan. “These screenings are an opportunity to provide the education and support these kids and teens need to stay healthy.” One of the main concerns LGBTQIA+ youth often have is that they will experience judgment from their provider, or the PCP will disclose sensitive information, including their sexuality or gender identity to their parents, when they are not ready to do so. Dr. Barangan emphatically reminds us that this legally cannot happen. “If a patient asks me to keep something confidential, unless they disclose that they have plans to harm themselves or others, I am legally not allowed to share that information with anyone without their permission,” said Dr. Barangan. 3. Locate Local Resources Northern Nevada is home to a variety of resources for the LGBTQIA+ community at large, including youth members of this community. "Finding resources to help them develop in a positive way and provide them with the information they need, whether it be in school, the household, the community or through a medical or mental health provider, is incredibly important,” said Dr. Barangan. Below is a list of local LGBTQIA+ community resources open to you and your children: Our Center LGBTQIA+ Health Services at Northern Nevada HOPES Northern Nevada Pride Festival & Community Parade (happens every July in Reno) Sassabration (happens every September in Carson City) Lake Tahoe Pride (events and resources shared on Facebook) © alessandrobiascioli via Canva.com
Read More About 3 Ways to Foster the Wellbeing of LGBTQIA+ Kids and Teens
-
Early Detection is Key to Surviving Colorectal Cancer
Colorectal cancer is the number two cancer killer in Nevada, only second to lung cancer, yet it is also one of the most preventable. Still, in 2020, 20.7% of Nevadans said they had never been screened for this deadly disease, according to the Nevada Cancer Coalition. At the start of the COVID-19 pandemic, unfortunately many healthcare services were halted, including colorectal cancer screenings. Those delays in screenings can lead to delays in diagnoses of colorectal cancer, resulting in poorer outcomes. Per the American Cancer Society, if colorectal cancer can be found early the relative 5-year survival rate is approximately 90%. Screening is key, and it is important to engage in preventative care. Even if you have no personal or family history of colorectal cancer, ask your doctor about colorectal risk factors and when to start screening, and if you’re up to date on your screenings, talk to loved ones and make sure they are too. According to the American Cancer Society, most colorectal cancer cases are found in those without a family history. This month let us help raise awareness for colorectal cancer and the importance of routine, life-saving screenings. To learn more, we spoke to Renown Health oncology nurse Christina Alsop, APRN. What is Colorectal Cancer Colorectal cancer is a disease in which the cells in the colon or rectum grow out of control. It usually forms from precancerous polyps, or abnormal growths, in the colon or rectum, which can become malignant without presenting any symptoms. How do Screenings Work Screening tests like stool tests, colonoscopies and others can detect these precancerous polyps, so they can be removed by a physician before turning into cancer. Screening tests can also find colorectal cancer early, resulting in better treatment outcomes. As of 2021, the U.S. Preventative Services Task Force recommends adults begin colorectal cancer screenings beginning at age 45, through 75. Screening methods include a blood stool test, which needs to take place every year or a colonoscopy, which takes place every 5-10 years. Healthy Habits Can Help Stave Off Risk Routine screenings are the only way to determine colorectal health, yet some healthy habits may reduce your risk for colorectal cancer. These factors include maintaining a healthy weight, being physically active, eating a diet rich in fresh fruits, vegetables and whole grains, limiting alcohol intake and not smoking.
Read More About Early Detection is Key to Surviving Colorectal Cancer
-
6 Healthcare Action Items for the LGBTQIA+ Community
Every patient, regardless of how they may identify, greatly benefits from preventive healthcare and early detection. Members of the LGBTQIA+ community face unique considerations when it comes to their health, and a proactive approach to preventive screenings and vaccines is important in order to address their individual health needs. Dr. Karen Thiele, Family Medicine Physician with University Health and Assistant Professor of Family and Community Medicine at the University of Nevada, Reno School of Medicine, breaks down key steps that LGBTQIA+ patients should take to safeguard their health. PrEP and PEP Pre-exposure prophylaxis (PrEP) is a strategy to prevent human immunodeficiency virus (HIV) infection. It is an important measure for those who are HIV-negative but may be at risk of contracting it. The highest risk sexual practice is receptive anal intercourse, due to the relative fragility of rectal tissue. This medication can stop HIV from spreading in the body and help patients maintain their HIV-negative status. PrEP is available in both pill form, which is taken every day, and injection form, of which the first two injections are initiated one month after another while all other injections are initiated every two months. Post-exposure prophylaxis (PEP) is an antiretroviral drug regimen taken after potential HIV exposure to prevent an HIV-negative individual from converting to HIV-positive status. PEP is only for emergency situations and must be started within 72 hours of exposure – sooner is always better than later – and must be taken for 28 days. PrEP and PEP are available in many ways, including visiting your primary care provider (PCP) or an urgent care location. HPV Immunization All genders and identities can protect themselves against human papillomavirus (HPV), a sexually transmitted infection (STI) that can lead to the risk of cervical, mouth, head, neck, throat, anal, vaginal, penile and vulvar cancers. HPV is so common that nearly all sexually active people, regardless of sexual orientation and practices, will be exposed at some point in their lifetime. The HPV vaccine (common brands include Gardasil and Cervarix) is a safe and effective method to prevent HPV, according to the Centers for Disease Control and Prevention (CDC). This vaccine protects against infections that can lead to HPV-related cancers and precancers, as well as genital warts. While patients should start receiving the vaccine at 9 years old years old, unvaccinated adults up to the age of 45 can also receive the vaccine through their PCP – better late than never!
Read More About 6 Healthcare Action Items for the LGBTQIA+ Community
-
Know when to visit an ER: Top 5 concerns
When a sudden illness or injury occurs, the emergency room (ER) provides immediate medical attention to those in need. Understanding the top reasons for visiting the ER can help people make informed decisions about seeking emergency care. Here are the five most common reasons people in Nevada visited an ER in 2023. 1. Abdominal pain One of the top reasons people visit the ER is abdominal pain. The abdomen has many organs, including the stomach, liver, small and large intestines, gallbladder and pancreas. Significant pain in this area can be a cause of concern. Warning signs of a serious problem include abdominal pain with fever, vomiting, and not being able to move or perform everyday tasks due to pain. Seeking medical attention when experiencing these symptoms is essential. Emergency physicians can perform abdominal exams, assess the condition and rule out significant threats. 2. Fever High fevers that do not get better with medicine and are accompanied by other symptoms can cause concern. This can indicate that the body is fighting off an infection or illness. Fever with symptoms like vomiting, pain, altered mental status, shortness of breath or inability to perform daily functions are warning signs to watch out for. Adults and children should visit an ER, where the team can assess the causes of the fever. 3. Chest pain and shortness of breath Chest pain and discomfort, or pain in the upper body can suggest warning signs of a heart attack. If a person is experiencing signs of a heart attack, call 911 immediately to ensure timely treatment or assessment by a medical professional. Heart attack symptoms include: Chest pain, including pain that can be described as chest pressure, heaviness or squeezing Discomfort in the chest, arms, back, neck, shoulders and jaw Difficulty breathing Sweating with any of the above symptoms When visiting a Renown ER for chest pain, a trained medical professional will promptly perform an Electrocardiogram (EKG) in an area where preliminary assessments, also known as triage, take place. Individuals experiencing shortness of breath or trouble breathing, whether from a respiratory infection, asthma complications or other pre-existing conditions should not ignore symptoms as these can signify more serious issues. Warning signs of respiratory distress may include: A significant change in breathing rate A significant change in the amount of energy used to inhale or exhale when breathing Changing of the skin color to blue, gray or paleness, which can indicate a lack of oxygen Nasal flaring Chest retractions, which can suggest difficulty bringing air into the lungs What this looks like: the chest sinking in just below the neck, breastbone or rib cage while breathing 4. Neurological symptoms Sudden and severe headaches or seizures may prompt individuals to visit the ER if symptoms are extremely disorientating or debilitating. These symptoms could be indicative of various conditions, including strokes or neurological disorders that require prompt evaluation. If a person is experiencing signs of stroke, call 911 immediately to ensure timely treatment. Stroke symptoms include: Numbness, weakness or loss of movement in the face, leg or arm, especially on one side Confusion, including trouble speaking or understanding Trouble with vision or loss of balance When choosing emergency care for signs and symptoms of stroke, a Comprehensive Stroke Center can provide patients with immediate intervention, including evaluation, treatment and education. 5. Cough/flu-like symptoms Emergency departments are staffed by medical professionals trained to prioritize and treat emergency and trauma situations. Receiving care at an ER should be reserved for severe symptoms and life-threatening conditions. It’s best to schedule a visit with a primary care physician for mild cold and flu symptoms. Most urgent care locations are equipped with rapid testing options, including RSV, COVID-19, influenza, mononucleosis, urinary issues and strep throat. It is critical to distinguish between common respiratory infections and more severe cases, such as pneumonia or complications from the flu. Symptoms that may warrant a visit to the ER include: Rapid decline in the ability to perform regular daily activities Coughing or throwing up blood Severe dehydration and inability to drink fluids High fever not responsive to medication Understanding top ER visits in Nevada While these ER complaints are common reasons for emergency room visits in Nevada, it's important to remember that emergency care is available for all immediate medical needs. Do not hesitate to seek help at an emergency room if someone experiences a sudden or severe health concern. Quick and appropriate action can make a significant difference in keeping you and your loved ones healthy. Renown Health is the largest locally governed, not-for-profit healthcare network in northern Nevada, providing leading emergency and trauma care by board-certified emergency physicians 24/7 at three locations, including the region’s only pediatric emergency department. Renown Health emergency rooms prioritize swift assessments, advanced diagnostic tools and compassionate care, providing leading emergency and trauma care. Trust Renown ER for not just emergency care but exceptional care. Learn more at renown.org/ER.
-
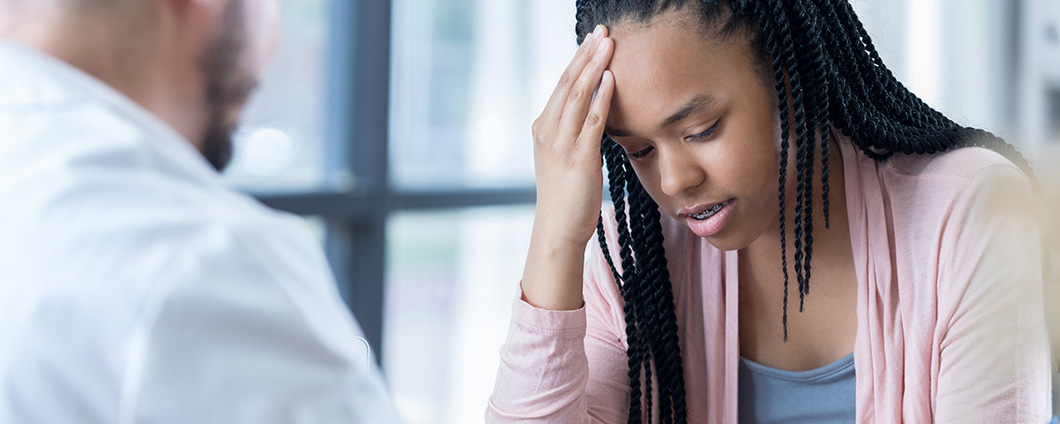
Headache Program
Renown Health's Institute for Neurosciences has expert physicians who provide compassionate diagnosis and care for chronic headaches & migraines and elevate the standard of care through clinical research and trials. Our physicians provide a pain-management plan tailored to your symptoms and provide follow-up pain management. If you don't have a primary care physician, we will provide one to help you along the way. To learn more about the Headache Program and Migraine Treatment at Renown Health, please call: 775-982-2970